Abstract
Introduction There is an increasing recognition of the need for deployed intensive care physicians (intensivists) with the changing nature of conflict. Required capabilities of military intensivists are determined by the operational context and is different to those of the civilian work environment. We sought to identify an operational clinical skillset for military critical care physicians.
Methods To answer the research question, we performed a literature review to identify existing intensive care competency frameworks and define the scope of practice for a deployed intensivist. Quantitative and qualitative research articles of any design were eligible for inclusion if the context included intensive or critical care medicine in a deployed environment. Articles were identified on PubMed, Medline, EMBASE, Google Scholar and EBSCO and included in the review if they met inclusion criteria.
Results Several quantitative studies described battle injury patterns and identified predominant mechanisms of injury. Deployed intensivists frequently have to manage patients with non-combat injuries and medical conditions. Paediatric patients also require ICU care in a deployed environment with high injury severity and in-hospital mortality.
We identified a subset of qualitative articles that described the general characteristics of military critical care patients; important considerations related to infections in a deployed environment and ethical and legal decision making.
Several articles discussed training and equipment considerations (including ICP monitoring, ultrasound and renal replacement therapy) in preparation for potential peer-on-peer conflicts.
Discussion The reviewed articles allowed us to identify the skills a deployed intensivist requires beyond the baseline civilian clinical skillset. We used this information to propose a core operational clinical skillset for deployed intensivists. This intends to help individual clinicians and commanders identify training pathways to prepare competent clinicians who are adequately prepared for military deployments
Introduction
Military health services aspire to provide best-practice care to those who become ill or wounded on operations. Historically, since the Vietnam War, military health support has prioritised rapid surgical intervention followed by early transport to definitive care. The application of damage control principles from the start of the 21st century led to recognising the need for intensive care physicians (intensivists) in forward hospitals to manage patients who cannot access timely retrieval, and to allow optimal management of high acuity disease non-battle injuries (DNBI).
The capabilities required of military intensivists are determined by the operational context, duration of deployment, retrieval system and specialist supports, among many other factors; however, it is likely that in many cases, the exigencies of deployed healthcare will call upon intensivists to work in unfamiliar ways. While work has been done to understand the training gap between civilian and military clinicians in surgical specialties,1 similar work for intensivists is less progressed. We, therefore, aimed to derive an operational clinical skillset (OCSS) for deployed intensivists to inform the maturation of the specialty in the military context.
Methods
The population of interest for our review was defined as military intensivists, and material relating to intensive care practitioners from other specialties was included. Only English language papers relating to developed world militaries that addressed the deployed setting were reviewed. Any study design was acceptable, including expert commentary. We used the search strategy outlined in Figure 1 to identify relevant articles in PubMed, Medline, EMBASE, Google Scholar and EBSCO.
Each paper was reviewed for relevance by two reviewers, with a third reviewer involved to resolve disagreements. Following inclusion, material of interest was entered into a research database. This material included content relating to (1) case-mix and case load for deployed intensivists, (2) required competencies of deployed intensivists, (3) required skills of deployed intensivists, (4) proposed training programs for deployed intensivists, or (5) pre-deployment training of military intensivists.
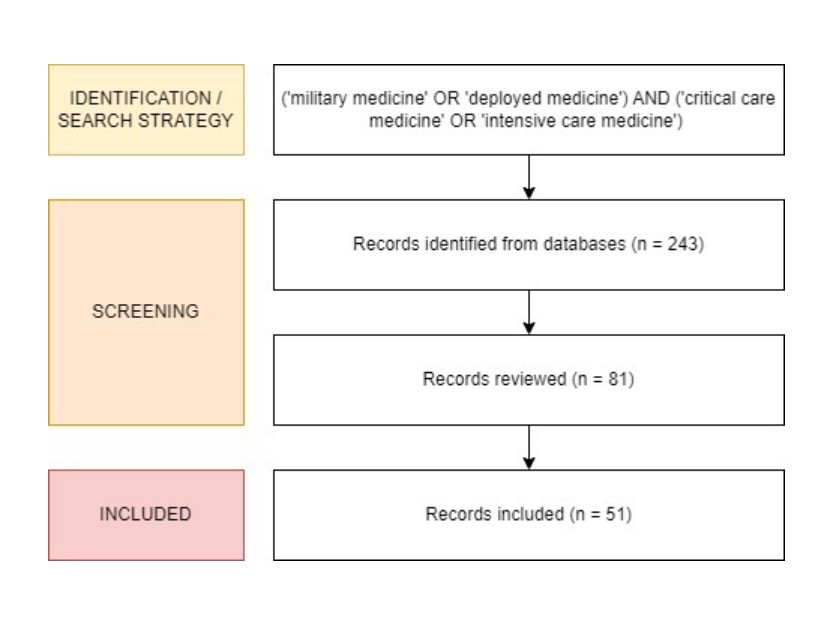
Figure 1: Search strategy and identification of relevant records.
Results
All quantitative studies describing case-mix and procedures in deployed ICUs were observational, retrospective analyses of medical records. Most focused on the conflicts of this century in Afghanistan and Iraq, although some reports addressed deployments in other conflicts, peacekeeping, and humanitarian assistance and disaster response (HADR). Studies are summarised in Table S1 (supplementary material).
Battle casualties are commonly caused by blast and gunshot wounds (GSW)
Several papers exclusively considered battlefield injury presentations to deployed hospitals. Reports were heterogeneous; however, a consistent finding was that blast injury and GSW were common. Widespread use of body armour has resulted in a higher proportion of severe pelvic, head and peripheral injuries.2 While most injuries treated in deployed facilities are minor (AIS=1; 74% minor injuries only; fatality rate 4.6%), patients with severe injuries frequently require critical care (e.g. 12% intubated and 4.6% requiring thoracostomies).3
In the Iraq war, 87% of casualties suffered blast injuries (49% to extremities and 36% to the head and neck).4 Similar rates of blast injury have been reported in Afghanistan.5, 6 Among blast casualties, primary blast lung injury (PBLI) was noted in approximately 10% of patients, often requiring mechanical ventilation in the ICU prior to transfer.7
Penetrating trauma remains common in military ICU patients, both from GSW and secondary blast injury.5, 6, 8, 9 Civilians and children are particularly prone to penetrating head injury.6, 9
Motor vehicle accidents (MVA) made a variable but significant contribution to presentations (2–19%).5, 8
ICUs in warlike settings must anticipate disease non-battle injury (DNBI) admissions
DNBI in warlike settings was investigated in two studies set in Iraq. A US study found a 6.1% ICU admission rate for patients presenting with DNBI to a Role 3 hospital,10 while a British study looking at presentations to a Role 3 facility with heat illness (n=622) described 15 patients who required ICU admission.11
Two studies investigated military and DNBI presentations together. Of patients presenting to a German Role 3 hospital in Croatia, 0.7% required ICU admission; 54% of these were for surgical indications and 46% for medical conditions.12 A more recent British study set in Iraq found that 27% of inpatients required ICU admission, and trauma was most common (83%); the medical ICU admissions were diverse and included similar presentations to what would be expected in a civilian ICU.13
DNBI presentations are diverse; deployed intensivists have reported management of myocardial infarcts, strokes, acute leukaemia, Guillain-Barre syndrome, Stevens-Johnson syndrome and exacerbations of chronic disease.14, 15 Complications of supplement use and alcohol-related illnesses may also be more common in deployed ICUs.14, 16
Presentations of pulmonary disease are emphasised in several papers. These include those routinely managed in civilian units and also location-specific infections (haemorrhagic fevers and clusters of Q-fever, Bordetella pertussis, Chlamydia, Mycoplasma and Acinetobacter), chemical and other inhalational injury, and clusters of acute eosinophilic pneumonia.17
The majority of ICU admissions during HADR are for non-traumatic presentations
Three studies specifically investigated HADR. An Israeli hospital deployed following an earthquake in Türkiye reported a 5.2% ICU admission rate, predominantly for medical illness (55.6%); only 7.9% were due to trauma.18 Similarly, of only two cases admitted to ICU in a UK hospital deployed in South Sudan, both were for infectious diseases.19 A hospital deployed following the Houston floods had a 3.2% ICU admission rate, although the nature of admission was not published.20
Infection and sepsis are common complications in deployed ICUs
Intensivists may face unfamiliar organisms and drug-resistance patterns, including biological weapons and potentially increased iatrogenic infection rates.14, 16, 17, 21-25 Multi-drug-resistant organisms are a common cause of combat wound infections.2, 26 This is complicated by the challenge of reduced diagnostic and drug concentration monitoring capability in deployed facilities.27
Deployed ICUs treat diverse patient populations and paediatric admissions are common
Military intensive care patients are generally younger and fitter than in civilian hospitals.16 However, in both warlike and non-warlike settings, non-military patients are commonly admitted to deployed ICUs.15, 16, 21, 22, 25, 27, 28 Presentations of local elderly and obstetric patients can also be expected.15, 16
A review of 9 years of data from Iraq and Afghanistan identified almost two-thousand paediatric ICU admissions to coalition hospitals, primarily for explosive (45%) or firearm (21%) injury.29 Inwald et al. reported that 14% of admissions to a UK-deployed ICU were aged under 16.30 Acuity of paediatric presentations to military hospitals is high. Of children presenting to a military emergency department in Afghanistan, 63% required admission to ICU.31 Another reported that 144 of 955 children (15.1%) presenting to deployed hospitals in Iraq and Afghanistan with thoracic injuries died.32 Further, Spinella et al. reported that 11% of patients requiring mechanical ventilation were children, and the in-hospital deaths for children were significantly higher than those for adults (5.4% vs 1.3%, respectively).33
A review of paediatric burn casualties that presented to US-deployed hospitals in Iraq and Afghanistan identified 549 patients. Just under a quarter (23.8%) had severe burns (TBSA 39-89% or 29% to 79% if age < 5 years). In this group, ICU utilisation was significant, with no ICU-free days (IQR 0-22) and six ventilator-free days (IQR 0-29) for survivors (52.7%).34
Military intensivists must be able to function in austere and hostile environments
While civilian intensivists are trained to work in situations of stress and high clinical acuity, the deployed intensivist must be able to provide care in the face of threats to personal safety, extreme fatigue and psychological stress.15, 25 There is also a need for military intensivists to contribute to triage and multi-casualty management.15, 16, 35
Deployed ICUs must operate in an environment characterised by reduced staffing, consumables, space, lighting, power, water and infrastructure.16 Diagnostic technology will not be equivalent to civilian institutions.39 Oxygen will not be unlimited; clinicians must be familiar with low-pressure oxygen equipment.15 Retrieval resources may also be limited, leading to long primary and secondary retrieval times and a higher proportion of patients affected by hypothermia, hypovolaemia, sepsis and psychological sequelae of prolonged field care.16
Deployed intensivists must allocate limited resources in accordance with established ethical and legal frameworks
Austerity also dictates that deployed clinicians must make decisions regarding the use of limited resources, including withholding care from severely injured casualties.15, 16, 28, 40 International humanitarian law and medical rules of eligibility determine which patient groups can access the military health system, clinicians must balance the needs of the wider military organisation with those of the individual patient.28, 39, 41 Treating severely injured local casualties poses ethical dilemmas regarding eventual discharge to the local health system, the ongoing management of newly diagnosed diseases, and the risk of creating a dependence on the military facility.14, 25, 28, 39-41
Civilian intensive care fundamentals remain important in the deployed setting, but military intensivists may need to adopt additional roles
In the deployed setting, fundamentals of routine ICU care remain essential, including DVT prophylaxis, nutrition, infection control, and cardiovascular and respiratory support.2, 15, 21 However, specialised military knowledge may also be required; for example, in many deployed environments there is a tangible CBRN threat and several papers advocate for formal CBRN training for deployed intensivists.16, 42, 43
Likewise, while civilian intensivists must attain competence in transfusion medicine, the deployed intensivist must have a detailed understanding of military blood stocks and supply chains, including products that may not be routinely available in their civilian practice, such as whole blood. They must also be able to make appropriate use of military-specific transfusion practices, such as the walking blood bank.14, 39, 44
Specialist imaging support may be limited, and point-of-care ultrasound, including focused abdominal sonography of trauma (FAST) and echocardiography, was identified as an important skill in several papers.14, 35, 39, 45
Similarly, while ICP monitoring was considered an essential skill by some authors,14 neurosurgical support may be remote or unavailable. Experience in rural UK civilian hospitals has shown that intensivists can be trained to insert ICP.39, 46
Prolonged care in deployed ICUs may necessitate additional clinical capabilities
Many treatments commonly employed in civilian ICUs are not used as often in the deployed setting due to resource constraints and the availability of timely evacuation.
One example of this is renal replacement therapy (RRT).39 However, higher casualty rates and longer evacuation times anticipated in future warfare may necessitate field RRT,47 including pumpless solutions such as arterio-venous filtration and peritoneal dialysis.
Similarly, enteral nutritional support is less commonly instituted in deployed ICUs, and parenteral nutrition is generally unavailable.39, 48, 49 As the availability of rapid evacuation cannot be assumed in future conflicts, the provision of more definitive nutritional support would be required.37
Deployed intensivists may encounter highly specialised interventions that are not a routine feature of their domestic practice
Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA) has been used in deployed hospitals, and a training package is described for its use.50, 51 Likewise, while Extracorporeal Membrane Oxygenation (ECMO) is not routinely available in deployed ICUs39 the Lung Assist arterio-venous ECMO device has been successfully used to stabilise and retrieve combat casualties.14, 52
REBOA and ECMO are likely to be used infrequently and these capabilities are expected to be facilitated by an external specialist retrieval team. Nonetheless, several case reports relating to these capabilities suggest that intensivists deploying to specified operational contexts should have a working familiarity with these interventions.
Specific training in intensive care is associated with improved patient outcomes in the deployed setting
A retrospective observational cohort study of a deployed military ICU found that the presence of a trained intensivist was associated with reduced mortality, duration of mechanical ventilation and ventilator-associated pneumonia.14, 53 Sattler describes an educational program to train deployed intensive care medical officers (not necessarily qualified intensivists) in identified critical skills. Of these, most would be considered routine intensive care procedures in Australia, the exceptions being paracentesis, tourniquet placement, ocular trauma management, splinting, laceration suturing, abscess drainage and mass-casualty management.35
Table 1. Skills that may be required of deployed military intensive care physicians. (ICP: intracranial pressure: RRT; renal replacement therapy; eFAST: extended focussed sonography of trauma)
| General intensive care management Manage nutritional support Manage infection control precautions Initiate and manage cardiovascular support Initiate and manage invasive and non-invasive respiratory support Manage pain arising from surgery, trauma or medical conditions Prepare patients for retrieval and interhospital transport |
| Trauma patient management Manage blast injuries, including primary blast lung injury Manage burns, including severe burns Manage penetrating and blunt traumatic brain injury Manage ocular trauma Manage thoracic trauma Manage extremity trauma Manage pelvic injury Manage complications of trauma (e.g. hypothermia, coagulopathy, sepsis) |
| Medical patient management Diagnose and manage a broad range of acute and chronic medical illnesses Manage heat injuries Manage alcohol- and other drug-related illness and intoxication Manage supplement use and contaminant toxicity Manage sepsis, including:
Manage ischaemic heart disease and cardiac arrhythmia in the absence of interventional cardiology support |
| Postoperative management Manage patients post-trauma and non-trauma surgery |
| Special patient groups Manage paediatric patients, especially:
Manage obstetric patients and complications |
| Leadership, personal and ethical decision making Work in stressful situations Lead others in stressful situations Work in austere and low-resource environments Triage and manage multi-casualty incidents Prioritise patients for secondary retrieval/strategic aeromedical evacuation. Crisis resource management Ethical and lawful decision making, including:
Adaptable to international teams/cultural humility |
| Procedural skills Perform routine ICU procedures, including:
Perform additional procedures, including
Initiate and manage improvised or deployable RRT
Manage deployed blood transfusion, including damage control resuscitation, resource management and walking blood bank management |
Discussion
This review sought to identify the training gap between the skillset of a conventionally trained Australian civilian intensivists and that desired of a deployed military intensivist.
In Table 1, we propose a core operational clinical skillset (OCSS) for the deployed intensivist based on our analysis of the historical case-mix and published expert opinion. Most of these skills would be fundamental to the deployed intensive care skillset, such as general intensive care patient management, blunt and penetrating trauma injuries management and the ability to perform common procedures. Specialised procedures would be performed by the intensivist only in the absence of other more experienced providers, for example, ICP monitor insertion. Additionally, some procedures identified in our review, such as REBOA and ECMO, have been excluded from the core OCSS because their use is infrequent and skill maintenance is likely impractical and cost-prohibitive. They may be employed in specific circumstances by smaller subspecialty teams.
The other side of the training gap is the baseline skillset of civilian intensivists. Most intensivists benefit from a comprehensive training program. This training program includes core skills, including the management of presentations commonplace in developed countries, a range of routinely performed procedures, and the management of advanced respiratory, haemodynamic and renal supports.
Other skills may be somewhat familiar to civilian intensivists, but their increased frequency or complexity on deployment may justify upskilling; for example, treatment of tropical diseases, trauma management and crisis resource management. Even core skill domains such as transfusion have unique military considerations, including the use of walking blood banks and frozen blood modules. Finally, several skills would be almost entirely unfamiliar and would require substantial training, such as peritoneal dialysis and ICP monitor insertion.
Likewise, while many intensivists are familiar with ultrasound and echocardiography, they may require upskilling in eFAST.
Notwithstanding the core domains of practice addressed by ICU training, the experience and skillset of intensivists vary significantly. To ensure competence and confidence in the deployed setting, each practitioner must identify individual learning needs after reflecting on the gap between their experience and the proposed OCSS. Additional gaps may exist if a deployed ICU is to be staffed with clinicians who have not completed specialist training in intensive care medicine.
Unsurprisingly, this review has identified trauma as being a common cause of admission to deployed ICUs. However, widespread use of body armour has somewhat reduced thoracic trauma, resulting in higher proportions of head, neck and extremity injuries. Burns are also more common than in most civilian units. A further important finding was that DNBI admissions are common in both warlike and non-warlike deployments. Several medical presentations were more common on deployment than expected; managing tropical and region-specific diseases may require significant upskilling for many Western-trained intensivists. Management of inhalational injury and CBRN casualties may be similar examples.
Despite military hospitals being intended to treat adults, paediatric ICU admissions were common across several studies. Intensivists who work in adult units may require refresher training on paediatric medicine. While equipment provision was not a focus of this paper, this finding has obvious implications regarding the equipment that a deployed ICU may require.
Finally, non-technical skills, including ethical and legal decision making, leading teams in high stress situations, and multi-casualty management, are areas where upskilling would be required for many intensivists. While some of the skills are fundamental to ICU practice, the specific scenarios, laws and ethical considerations encountered on deployment are likely to be unfamiliar to a civilian intensivist.
The authors were surprised by the lack of one result in particular. In our experience, the intensivist is often called upon to manage medical presentations that do not need intensive care but do not fall within the specialty domains of other deployed medical officers (in the absence of an internal physician). Management of acute coronary syndromes would be a typical example.
With the intensive care OCSS defined, the next task is identifying pathways by which individuals can achieve competence prior to deployment. Solutions may include hospital placements with specialty practice areas, such as trauma, burns and paediatrics. Even within trauma centres, Australia has low rates of penetrating and blast trauma presentations, so overseas placements may be effective. There may be a role for specialty courses, such as tropical disease intensives and ethical decision-making scenario training.
Limitations
There are two key limitations of this study. Firstly, there was significant heterogeneity between studies, presumably due to regional variations in practice. ICU admission rates varied significantly. Similarly, among the qualitative papers, assumptions regarding baseline skillsets of intensivists may have varied depending on the system in which the authors trained and worked.
Secondly, most of the papers identified in this review examined experiences from the Iraq and Afghanistan wars. These conflicts were characterised by low-tempo asymmetric warfare, relatively small numbers of severely injured casualties, and coalition air superiority, allowing rapid evacuation. Future wars may not share these characteristics; severely injured casualties may be more frequent and unable to be moved rearward in a timely manner.36, 37 Even communication and telehealth, heavily relied upon in recent conflicts, may not be available in the next.38
Conclusion
This review has allowed us to derive a preliminary OCSS for intensive care. This document will allow individuals to prepare themselves more effectively for their deployed role, and allow commanders and managers to weigh the risks and benefits emerging from the decision to employ non-specialist intensive care providers in specific operational contexts. Future work should seek to map out operational clinical readiness pathways that support individuals in closing the gap between their civilian experience and the demands of deployed intensive care.
Corresponding Author: Adam Mahoney, adam.j.mahoney@gmail.com
Authors: A Mahoney1,2, J L Begley1,3, M Reade1,4, F Pracher5,6
Author Affiliations:
1 Australian Army – 2nd Brigade
2 Royal Hobart Hospital
3 The Alfred
4 University of Queensland – Burns, Trauma and Critical Care Research Centre
5 Townsville Hospital and Health Service
6 Royal Australian Air Force – Health Services Wing


