‘Military Superbug’ Acinetobacter Baumanii Induced Sepsis in Craniofacial Gunshot Injuries
I Danish Khan, Associate Professor, Army College of Medical Sciences and Base Hospital, New Delhi, India
Craniofacial gunshot injuries encountered during CI/CT operations are involved in a situational complexity requiring astute battlefield care, streamlined evacuation logistics, and operative and critical life support capabilities at various echelons along the chain of evacuation.Secondary infections by ‘military superbug’ Acinetobacter baumanii complicating to sepsis can jeopardize survival.The discussion is focused on two combatants who sustained craniofacial gunshot injuries during CI/ CT operations in hilly jungle terrain of South- Asia.Having survived through initial assault of the gunshot and initial resuscitation, they were tactically evacuated on ventilator support to tertiary care facility located more than 1800 km from site of injury in South-Asia.In the backdrop of tissue devitalization, hemodynamic and renal compromise, extensive surgical and critical care interventions,
Abstract
Background Craniofacial gunshot injuries encountered during counter-insurgency/counter-terrorism operations are involved in a situational complexity requiring astute battlefield care, evacuation, operative management and critical life support.Secondary infections by ‘military superbug’ Acinetobacter baumanii complicating to sepsis can jeopardize survival.
Cases Two combatants sustained craniofacial gunshot injuries during counter-insurgency/counter-terrorism operations in hilly jungle terrain of South-Asia.Having survived through initial assault of the gunshot and resuscitation, they were tactically evacuated on ventilator support to tertiary care.In the backdrop of tissue devitalization, hemodynamic and renal compromise, extensive surgical and critical care interventions, secondary infection by multidrug resistant Acinetobacter baumanii led to sepsis and demise.
Conclusions Craniofacial gunshot wounds in the battlefield can initiate a domino effect leading to physiological complications which can predispose to secondary infections, leading to sepsis and demise.Acinetobacter baumanii known to survive in environmental reservoirs, can cause bacteremia and sepsis in gunshot, warfare injuries and natural disasters.A prudent emphasis on secondary and opportunistic infections in battlefield and hospital care is mandated to optimize outcome in gunshot injuries.
Key Words gunshot, ballistic trauma, Acinetobacter baumanii, military superbug, sepsis
Introduction
Guns and assault rifles have been indispensable weaponry from medieval to modern era. Gunshot injures cause gunpowder propelled projectile-induced penetrating ballistic polytrauma. Gunshots comprise 50-90% of injuries encountered during low-intensity conflicts, civil wars and counter-insurgency/counter-terrorism (CI/CT) operations.1 High velocity (1500 m/sec) rifled gunshots are commonly encountered among soldiers fighting belligerent guerillas in CI/CT operations in contrast with low velocity (350-500 m/sec) pistols used commonly in civil wars. High velocity rifled gunshots produce heavy craniofacial damage to vital neuromuscular structures from passage of missile, secondary shock wave and cavitation, despite smaller entry wound. In addition, they pose a higher risk of infection.2,3
The incidence of gunshot injuries in US and Indian Armed Forces is 0.34-0.68/1000 person-years and 1.07/1000 troops respectively.3,4 The incidence of gunshot injuries was 53.5% during terrorist attacks, armed banditry and communal clashes in Nigeria, 91.8% during Boko Haram insurgency and 72.2% during Libyan Civil War insurgency.5,6 US and UK military data reveal significantly higher mortality secondary to gunshot compared to explosions.7,8
Craniofacial gunshot injuries encountered during CI/CT operations are involved in a situational complexity requiring astute battlefield care, streamlined evacuation logistics, and operative and critical life support capabilities at various echelons along the chain of evacuation. Secondary infections by ‘military superbug’ Acinetobacter baumanii complicating to sepsis can jeopardize survival. The discussion is focused on two combatants who sustained craniofacial gunshot injuries during CI/ CT operations in hilly jungle terrain of South- Asia. Having survived through initial assault of the gunshot and initial resuscitation, they were tactically evacuated on ventilator support to tertiary care facility located more than 1800 km from site of injury in South-Asia. In the backdrop of tissue devitalization, hemodynamic and renal compromise, extensive surgical and critical care interventions, there was secondary infection by multidrug resistant (MDR) Acinetobacter baumanii leading to sepsis and demise.
Case 1
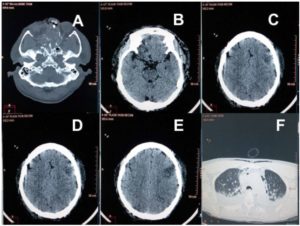
Fig 1 (Case 1: Gunshot wound Face): Non-contrast Computed tomography (NCCT) head revealing (A) Multiple skull fractures including fractures of maxillary antrum, nasal bone, ethmoid and sphenoid; (B and C) Cerebral contusions in bilateral basi-frontal, right anterior and high frontal lobes; (D and E) Contusion in left temporal and occipital lobes; (F) NCCT chest revealing bilateral pleural effusion, basal consolidation and pneumomediastinum.
A 52-year-old combatant sustained craniofacial gunshot injury over face and right eye during a CI/ CT operation. He was air evacuated to secondary care, where emergency tracheostomy, emergency repair of perforated posterior pharyngeal wall, lacerated tongue, evisceration of lacerated right eye, debridement of right open-globe injury, with packing of pharynx and primary repair of facial wounds was done. Continuous haemorrhage from oral cavity led to massive transfusion with 22 units whole blood within 48 hours of injury.
He was air evacuated on ventilator support to a tertiary care facility on the third day post injury for definitive management of fractured maxilla and palate, right open-globe injury, pharyngeal wall injury and a suspected splinter induced vascular injury on left side of neck. The Glasgow Coma Scale (GCS) was 7/15 with improving revised trauma scores. Noncontrast Computed Tomography (NCCT) of head revealed multiple fractures of skull, maxillary antrum, nasal bone, ethmoid and sphenoid, and cerebral contusions in bilateral basi-frontal, right anterior, high frontal, left temporal and occipital lobes. NCCT of chest revealed bilateral pleural effusion, basal consolidation and pneumomediastinum (Figure 1).NCCT of the cervical spine revealed multiple metallic foreign bodies in the neck with a large hematoma in the left parapharyngeal space. Computed tomography angiography revealed normal carotids. On the fourth day post injury, evacuation of the neck hematoma, re-packing of the oronasal and orbital cavity were performed followed by feeding via tube gastrostomy and jejunostomy. His left eye revealed optic disc hemorrhage.
Blood culture revealed multidrug resistant Acinetobacter baumanii on the sixth day post injury for which colistin was initiated. On 12th day post injury, he developed hypotension, bilateral basal crepitations, decreased breath sounds due to pleural effusion with basal lung atelectasis, as revealed on contrast-enhanced computed tomography (CECT) of the chest. Features of sepsis with toxic granules, serum procalcitonin 40 ng/ml and sepsis induced delirium were noted. On day 16 post injury, he developed 104ºF fever with respiratory distress. Right lower lobe consolidation and bilateral pleural effusion were seen on a chest X-ray. His condition continued to deteriorate with deranged renal parameters, reduced urine output and increased dependence on inotropes. Urea and creatinine increased to 154 and 3.7 mg/dl respectively, and serum sodium and potassium reached 4.6 and 9.5 mmol/L while other hematology and clinical chemistry parameters were within normal limits. He succumbed to cardiac arrest on day 24 of injury. The cause of death was pneumonia and sepsis with multiorgan dysfunction.
Case 2
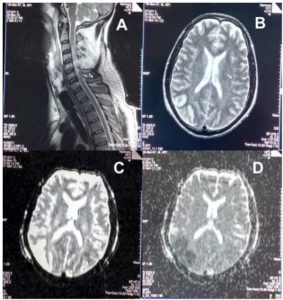 Fig 2 (Case 2: Gunshot wound Neck): Magnetic resonance revealing (A) Comminuted posterior fracture of C4 and C5, cord compression and edema extending from C3 to C6 vertebrae (B-D) Watershed infarct of right middle and posterior cerebral arteries, and occlusion of internal carotid artery.
Fig 2 (Case 2: Gunshot wound Neck): Magnetic resonance revealing (A) Comminuted posterior fracture of C4 and C5, cord compression and edema extending from C3 to C6 vertebrae (B-D) Watershed infarct of right middle and posterior cerebral arteries, and occlusion of internal carotid artery.
A 48-year-old combatant sustained gunshot injury at the angle of right mandible involving the face and neck in a CI/CT operation. He was resuscitated from hypovolemic shock, cardiac arrest and initiated on mechanical ventilation. Evaluation of the head and neck through NCCT and magnetic resonance imaging revealed cerebral oedema, watershed infarct of right middle and posterior cerebral arteries, occlusion of the internal carotid artery, cord compression and cord oedema, comminuted displaced fracture of right mandible and comminuted fracture of C4 and C5 vertebrae.(Figure 2) He was air evacuated on ventilator support under sedation to a tertiary care facility the same day where his GCS was E1VETM1 (sedated) with bilaterally sluggish pupils and quadriplegia.
Exploration revealed a laceration of the cord at C5 with large dural cord oedema. While he was being managed with inotropes, mannitol, dexamethasone, cefotaxime, amikacin and blood transfusion, he developed left lung consolidation and left pleural effusion. Intercostal drainage of 700 ml sanguineous pleural fluid revealed 250 leucocytes/mm3, lymphocyte predominance, 4 mg/dl proteins, 20 mg/dl albumin, 134 mg/dl sugar and 200 U/LDH. Tube feeding via gastrostomy and jejunostomy was initiated. Initially discouraging Trauma and APACHE II scores improved in intensive care.
During the course of his illness, leucocytes varied from 7000-25000/mm3, alkaline phosphatase 48- 311 U/l, urea 39-98 mg/dl and creatinine 1.4-1.9 mg/dl. Other parameters were within normal limits. His condition continued to deteriorate further with a low GCS, persistent fever, gasping respiration, hypotension requiring inotropes, decreased air entry bilaterally, neutrophilic leukocytosis with left shift, and high urea and creatinine levels. Tracheal cultures and blood cultures revealing MDR Acinetobacter baumanii. Serum procalcitonin levels reached 28 ng/ml despite the initiation of colistin. He succumbed to cardiac arrest on the 26th day post injury. The cause of death was sepsis due to MDR Acinetobacter baumanii.
Discussion
Gunshot wounds in the battlefield/operational scenario are severely damaging and lethal. Only 10% of patients survive to reach a medical facility.1 Battlefield healthcare principle of Tactical Combat Casualty Care is enmeshed in a situational complexity demanding overlapping operational parallels between medical and combat commands. Evacuation logistics affected by host conditions, terrain features, inclemency of weather, air capability, communication support and infrastructural limitations act as a caveat to the concepts of ‘Platinum half hour and Golden Hour’. Trauma scoring and stabilisation of the patient to cater for long periods of evacuation is critical. Mountainous and forested/jungle terrain restricts evacuation on foot by stretcher bearers till road-head or landing ground can be reached. Air effort for casualty evacuation is restricted by visibility, weather phenomenon and enemy action.9,10,11 It takes many hours for the patient to reach a facility where Damage Control Surgery and Damage Control Resuscitation can be offered as seen in these patients who had to travel hundreds of kilometers on ventilator support for definitive management.2,12,13
Gunshot projectiles crushing through tissues in ballistic penetrating trauma cause massive tissue devitalization, ischemia, anoxia and coagulopathy, and increased susceptibility to infections. Craniofacial gunshot injuries lead to an immediate deterioration of trauma scores, yet the benefit of doubt and/or opportunity should be given to the soldier. Given the high lethality of craniofacial gunshot injury, both patients survived for more than 23 days due to vigorous resource-intensive efforts, although they succumbed to secondary infection by the ‘military superbug’ Acinetobacter baumanii. Pharyngeal injury and neck hematoma, seen in the first patient, can lead to airway compromise and demise, which is a common complication of complex craniofacial injuries. During Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF), craniofacial gunshot injuries led to 67% fatal airway and vascular injuries, multiple facial fractures and airway haemorrhage.14 The second patient developed infection, respiratory distress and acidosis, which is known to occur in 3-10% of trauma patients.15 The incidence of infection in ballistic polytrauma remains at 35-40% despite surgical debridement and empirical antimicrobials.14 Uncontrolled haemorrhage even after surgery is attributable for 30-40% trauma related deaths .Massive transfusion is required in approximately 8% military casualties compared to 3% civilian casualties .The ‘Golden Hour Container’ utilizing phase-change materials can maintain temperatures for transportation of blood components without using electricity, batteries or even ice.8,11,16
Infections complicating to sepsis are considered potentially survivable.1,3,7,9 During the Soviet- Afghanistan War, the incidence of wound sepsis was 5.4% with 9.3% survival.17 Sepsis lead to 15.51% and 37.7% respectively from gunshot injuries in the Syrian Civil War and the Philippines.3,18 Tactical situation has played an important role vis-à-vis sepsis in predicting the survival from gunshot wounds throughout history.1,2,19
Both patients developed Acinetobacter baumanii infection despite being on empirical antimicrobials initiated at primary care. Acinetobacter baumanii emanates alarm at three axes. One, it is a robust pathogen found in soil and water at varied temperatures and thus can grow in land/water sources present in battlefields. Two, Acinetobacter baumanii being an emerging pathogen in battlefield injuries, may not be covered under clinical suspicion. Three, most Acinetobacter baumanii are MDR requiring aggressive reserve antimicrobials such as colistin or tigecycline, which may not be available at primary care. Acinetobacter can also exist in an immunocompromised host along with coinfecting pathogens.20,21,22
MDR Acinetobacter baumanii is known to cause bacteraemia and sepsis in gunshot and warfare injuries. The infection can be acquired in the battlefield or nosocomially in any echelon of care, given the ubiquity of the nonfastidious pathogen. Extensive tissue devitalization and systemic deterioration leads to an immunocompromised state furthering Acinetobacter induced sepsis which has a negative prognosis with 20-60% mortality.23 While susceptible Acinetobacter strains were isolated from Vietnam War injuries, 100 cases of MDR and two panresistant Acinetobacter blood stream infections meeting the CDC’s National Nosocomial Infection Surveillance criteria, were seen during OEF and OIF.Acinetobacter, quoted as the ‘military superbug’ and ‘Iraqibacter’, has now been included under the US Military ‘Global Emerging Infections Surveillance’ program.24,25,26 The risks of infection remains several weeks post-craniofacial ballistic trauma. MDR Acinetobacter entail aggressive empirical management and warrant usage of reserve antimicrobials such as tigecycline and colistin ab initio, which is against the existing guidelines of empirical antimicrobial therapy.27,28,29 Both tigecycline and colistin need to be given in sepsis dosage which renders patients prone to nephrotoxicity, neurotoxicity and gastrointestinal disturbances.
While the future of craniofacial trauma management may encompass haemostatic devices, lyophilized plasma30, walking blood banks31, and battlefield surgical robots32, a high index of suspicion is warranted toward emerging infectious diseases caused by Acinetobacter which can adversely affect patients improving from polytrauma. Advances such as tissue factor pathway inhibitor, tumour necrosis factor antibody fragment, platelet-activating factor acetylhydrolase, antithrombin III, pyridoxylated haemoglobin polyoxyethylene, mass spectrometry, MicroRNAs, proteomics and inflammmationomics can facilitate early diagnosis and intervention in infections and sepsis.33,34 An impetus toward damage control must include infection control in the conundrum of trigger-triggered complication cascade.
Conclusion
Craniofacial gunshot wounds in the battlefield can initiate a domino effect leading to pathophysiological complications from battlefield to tertiary care, such as projectile-induced penetrating ballistic polytrauma, haemodynamic and renal compromise, delayed evacuation, multiple critical care and surgical interventions, massive transfusions and tissue devitalization, which can predispose to secondary infections leading to sepsis and demise. Acinetobacter baumanii known to survive in environmental reservoirs, can cause bacteraemia and sepsis in gunshot, warfare injuries and natural disasters. A prudent emphasis on secondary and opportunistic infections in battlefield and tertiary care is mandated to optimize outcome in gunshot injuries.
Conflicts of Interest
None
Corresponding Author: Lt Col Dr Inam Danish Khan, titan_afmc@yahoo.com Authors: Inam Danish Khan1, Rajiv Mohan Gupta2, Sourav Sen3, Ajay Kumar Sahni3, Shazia Khan3, Ashok Kumar Jindal3, Bhaskar Mukherjee3, VK Sashindran3, Syed Asif Hashmi1, KS Rajmohan1
Author Affiliations:
1 Army College of Medical Sciences, New Delhi, India
2 Army Hospital Research and Referral, New Delhi, India
3 Armed Forces Medical College, Pune, India






