Republished Paper Captain Art Smith USNR attended and spoke at the 2005 AMMA Conference in Launceston. The following paper arose out of his
workshop and was initially published in the Naval War College Review. It is here reprinted with the Editor’s kind permission.
Arthur M. Smithb and Captain Harold R. Bohmanc
Medical support of the sick and wounded is a complicated, resource intensive, and vital aspect of any over-the-horizon operation. It
needs to be considered as a major subordinate command element just as the Ground Combat Element, the Air Combat Element and
the Combat Service Support Element are.
A NAVY COMBAT SURGEON
During World War II it took the Navy and Marine Corps years to confirm and refine their pre-war doctrine for amphibious attack. The labour began with the first U.S. landings at Guadalcanal in August 1942; the resulting doctrine, organization, tactics, and techniques were subsequently used by the Army in Europe. Early operations in both theatres highlighted the enormous difficulties associated with essential medical elements, and it was not until late 1944, perhaps 1945, that these problems were adequately solved. During future major expeditionary operations, will it take that long for a latent functionally effective medical support system to evolve? Will medical support of the anticipated “sea base” concept of operations, for example, be obligated to recapitulate the same sad evolution of repetitive mistakes committed during prior conflicts over the past century? It is imperative that those who bear responsibility for ensuring that prompt and competent care is provided to the combat injured examine the lessons emerging from historical precedent. Likewise, it would be reasonable to consider the “revolutionary” concept of establishing a “medical command and control element” in joint expeditionary operations, to obviate the often-validated reality that those who choose to ignore the lessons of history are destined to
repeat them.
In late 1992, the Navy formally shifted the focus of its planning from a Cold War scenario for opposing Soviet naval forces in mid-ocean toward a concept of countering land- and sea-based forces of potential regional aggressors in heavily defended littorals. It moved the focus of Navy
planning from a geographical environment where the force would operate primarily by itself to one of joint or combined expeditionary/amphibious warfare from a sea base independent of any land-based logistic lodgement. Today, in attempting to transform itself to meet twentyfirst- century needs, the Navy is emphasizing not only increased readiness but also the ability to deploy naval forces quickly in response to crises and conflicts around the world, notwithstanding homeland defence needs.
Since every option for transformation involves human assets, the potential for sickness and injury must be factored into any operational equation. From a medical perspective, a series of questions need to be answered, such as what specific forms of threat conjoined joint medical forces will likely face, and what role Navy medical resources will play in enabling the rest of the joint/combined force. What are the specific medical readiness goals for Navy medical assets functioning in a joint environment, and what resources will be necessary to reach them? Concurrently, what form of information
architecture will be required? Who, in the final analysis, will be responsible for ensuring compliance with goal expectations? Historical evidence of dysfunctional medical support during the last century of conflict is profoundly discouraging; some medical command and control mechanism in such joint/combined operations will be necessary to ensure functional compliance with readiness and operational objectives. Let us look first at the operational future.
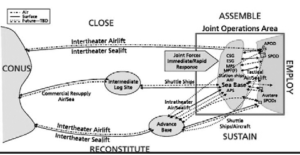
SEA BASING AND ITS PROPOSED MEDICAL SUPORT
A series of innovative proposals followed the adoption of the sea-base concept. New naval formations, such as the expeditionary strike group (amphibious ships combined with surface combatants, attack submarines, and land-based P-3 maritime patrol aircraft), were implemented. It has also been proposed to launch expeditionary operations, complete with command, control, and support infrastructures, directly from sea bases, to be formed, without necessarily establishing an intermediate land base, by a combination of amphibious and sealift-type ships. (The sea-basing concept responds to a concern that fixed overseas land bases in the future will become increasingly vulnerable to enemy antiaccess/area-denial weapons such as cruise missiles and theatre range ballistic missiles.)1 Computer technology will potentially tie together the personnel, ships, aircraft, and installations of the sea base in a series of highly integrated local and wide-area networks capable of rapidly transmitting critical information, under the rubric of “network-centric warfare.” An additional key program relating to sea basing is the notional Maritime Prepositioning Force (Future), or MPF(F), ship, which would replace the Marine Corps’s current “black bottom” maritime prepositioning ships operated by the Military Sealift Command utilizing civilian mariner crews. The MPF(F) ships are to be specifically designed to support the sea base while under way. Implementation
of the sea-basing concept will also possibly affect integration with future ships of the San Antonio (LPD 17) class of amphibious dock landing ships (which are replacing the old LPD types and five older LSD-36 dock landing ships) as well as the LHA Replacement (LHAR) program meant to retire the older Tarawa-class amphibious assault ships. Furthermore, it is anticipated that the legacy T-AH hospital ships will be replaced by a medical support system incorporating advancedlevel medical facilities within the MPF(F)s and the expeditionary strike group.
Under current consideration is the operational expectation that the component parts of a sea base could “close”—arrive and begin operation—anywhere in the world’s oceans within ten days of the executive order, by strategic air and sea lift, to be followed overnight by the insertion of two battalions of an expeditionary brigade into an operational objective, one by air and another by sea, all without any formal logistical support lodgement
ashore. The goal is to complete the entire “ship-toobjective manoeuvre” within thirty days. The return of the force to the sea base (“retrograde reconstitution”) would take an additional thirty days. The seagoing platforms of the sea base would comprise the ships of an expeditionary strike group and a carrier-based strike group, united with ships of the Maritime Prepositioning Force. The assemblage would sustain ground, sea, and
air operations with logistic support, command, control, communications, computers, intelligence, surveillance, and reconnaissance. It is envisioned that MPF(F)s themselves will meet all logistic requirements, including berthing for over sixteen thousand personnel, as well as extensive medical modules with surgical-specialty capabilities (known as “echelon level three” care). The medical modules would operate under “established
hospital standards of care,” utilizing appropriate nursing operating procedures. They would require specialized and trained personnel, equipment, and quantities of supplies as necessary to match the operational exposure of combat personnel.
Under the sea-basing blueprint, a ground combat component inserted ashore would have a minimal “footprint,” including a minimal medical support
structure. It might be augmented by forward resuscitation and surgical (FRSS) units or some functional equivalent, providing limited surgical capability beyond that intrinsic to operational battalions. Even so, the limited depth of medical resources ashore will mandate prompt evacuation for the bulk of casualties—generally by air, or when required by high-speed seagoing “connector” vessels—to the ships of the sea base, primarily the
ships of the expeditionary strike group and MPF(F)s. If afloat resources are to be continuously available for new casualties, there will have to be an additional mechanism for evacuating initially treated casualties from the sea base to higher-level medical facilities, perhaps thousands of miles away.
An important question is: Will it work?
HISTORICAL MEDICAL LESSONS FOR SEA BASING
Gallipoli
History has adjudged the British attempt to take the Dardanelles at Gallipoli to be an amphibious fiasco, a failure owing in large degree to a lack of coordination between attack and supporting elements, including the medical services. Among the many medically related issues was the paucity of medical communications and a poorly coordinated mechanism for transfer of casualties out to ships, many of which were scarcely able to care
for them, if at all. Many deaths ensued, as did profound morbidities. The implication today for the likely result of poor coordination of medical assets under the sea-base concept is obvious.
On 26 April 1915 Surgeon General Birrell, director of medical services for the combined attack of the British and the Australian and New Zealand Army Corps (ANZAC), requested that he and his deputy be allowed to join the general headquarters on board the battleship Queen Elizabeth, where the operational commander was, to supervise casualty evacuation. His request was refused, and he was embarked instead on board Arcadian, a ship that possessed neither wireless communications with the shore nor medical assets.
On 28 April Birrell was sent the message: “Lutzow [a transport being used as a hospital transport ship] filling up rapidly. Request name of next hospital ship. Where is the advanced depot of medical stores? Running short of supplies.” Another message read, “Wounded arriving rapidly—about 500. Probably require another hospital ship.” To these messages there was no reply. The director of medical services never received them. He was isolated—all signals from shore were conveyed by wireless to Queen Elizabeth, where the general’s staff, which was supposed to be coordinating the wounded evacuation, remained silent.2
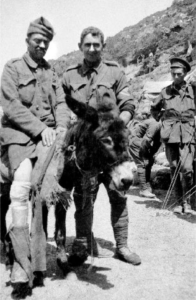
Private John “Simpson” Kirkpatrick and his donkey “Murphy” evacuating casualty with leg wounds, Gallipoli
Australia War Memorial, J06392
Casualties were transported to the beach on the backs of pack animals, as immortalized in ANZAC legend by the donkey “Murphy” and his bearer Private “Simpson” Kirkpatrick (see photo). These animals were variously led by members of irregular groups, such as expatriate European Jews (many driven by the Ottomans out of Palestine to Egypt) organized by the British into transportation units known collectively as the “Zion
Mule Corps”d.
The great numbers of Commonwealth casualties practically stopped operational activity on the beaches, and the devastation these drovers found at the water’s edge was graphically described by Colonel John L. Beeston of the Royal Australian Medical Corps: “The whole beach is filled with wounded of all kinds and descriptions. It has quite unnerved me for a time. Some of the wounds are so ghastly, whole abdomens blown away and the men still living. They are in such numbers that it is difficult to get along, and there is only one hospital ship in the bay.”3
At least twenty-two converted “hospital ships,” twenty troop ships, and other transports and merchant ships had been set aside for the reception of sick and wounded, but fear of Turkish coastal artillery and German submarines prompted many of these vessels to lie well offshore or in island ports some distance away. From the beaches, casualties were towed seaward in small craft, each carrying thirty patients, often in a frantic search at night for a ship to accept them. Concurrently, as troopships landed their complements on the beaches or transports unloaded their cargoes, they were rapidly filled with casualties. These “carriers” then moved to the hospital ships or other vessels lying offshore and likewise transferred the casualties
at sea, under occasionally difficult, even dangerous, conditions. As described by one historian, “the wounded were evacuated in large horse barges with sterns that could be let down for easy access; stretcher cases were placed in big boxes and hoisted into ships with the aid of derricks.”4 Some were swung on board by means of cargo nets dropped over the side.5 At a later stage, minesweepers partially fitted for medical purposes
were brought into use for evacuating casualties, and the British Red Cross provided six motor launches specially equipped to tow barges from the Gallipoli beaches (see photo). Ultimately, the large number of casualties at Gallipoli led to overcrowding, rendering many ships unsuitable as base hospitals. They became, in essence, casualty-clearing stations, providing interim and often merely token treatment of patients. The more serious
cases were transferred to distant shore bases in Egypt, Malta, and in some cases England itself.
Could the casualty-management breakdown witnessed at Gallipoli occur again under the modern banner of sea basing? Will a proposed diminution
of medical assets (a “reduced medical footprint”) accompanying expeditionary forces inserted from sea bases allow critical, life-threatening wounds to be attended to adequately? If all that is available ashore is a meagre casualty-sorting capability, and no efficient medical regulating network is established, will the results be any different from those experienced at Gallipoli?

Seaward evacuation of wounded by barge from Anzac Cove, Gallipoli.
Australia War Memorial, C02679
The U.S. Invasion of Grenada
On 21 October 1983, with the designation of Commander Joint Task Force 120, intensive operational planning was begun for Operation Urgent Fury.
However, no combat support planners, including medical representatives, were invited to participate. Consequently, no estimate of logistical supportability was completed prior to execution, and the required medical support system did not develop. The short lead time and the absence of a designated task force surgeon to coordinate medical services at the joint level left each service to plan medical support within the scope of its
own organic assets, with little or no joint coordination of such activities as casualty care management, whole blood procurement, and aeromedical evacuation. Erroneous assumptions may have been made as well. For example, the commander of the 82nd Airborne Division was informed that two amphibious ships, USS Guam (LPH 9) and Trenton (LPD 14), which were in the vicinity of Grenada, could provide significant medical and surgical support. The record is unclear, but this inaccurate information may have been responsible for his ultimate decision to keep Army medical support to a
minimum.6
The hostilities lasted ninety-six hours—123 casualties and eighteen deaths were recorded—and brought combat wounded to both Guam and Trenton. No significant or sustainable tactical medical asset was established within the combat zone during the hostilities, nor were there triage facilities ashore. Without trained and experienced triage corpsmen or officers, casualties were not sent in an orderly and logical flow to the proper receiving facilities. There were no established medical communication nets between the Army and Navy, let alone with Trenton and Guam; Army helicopter pilots, unfamiliar with the Navy ships and their silhouettes, brought casualties to whichever flight deck was most convenient. On several
occasions the better-equipped Guam was overwhelmed with both minor and lower-priority delayed casualties, while Trenton, which had no surgical capability, laboratory, or blood bank, was sent critical casualties. In essence, medical assets were squandered and overutilized simultaneously.7
Beirut 1983
The U.S. Marine compound at the Beirut International Airport was bombed on 23 October 1983. The tragedy presented an opportunity to evaluate in
detail the American military medical system’s ability to react to such incidents or, by extension, to a larger conflict. Among the principal components tested that day were medical command and control, casualty evacuation, medical regulating procedures, capabilities of facilities,joint medical readiness mechanisms, and the transition from routine peacetime to contingency operations.
A medical review group chaired by Rear Admiral James Zimble later evaluated the medical response to the bombing. Its 1984 report detailed serious deficiencies in medical readiness, attributing them in large part to a lack of medical evacuation resources, shortages of equipment and personnel, and inadequate joint planning for wartime or contingency requirements. The problems, it found, were also the result of the low priority habitually assigned to medical readiness in the planning, programming, and budgeting processes. As the report declared, “Had the ratio of killed-outrightto-
wounded been reversed, so that over 200 casualties had required treatment, rather than fewer than 100, the medical system might well have failed.” The report recommended greater investment in essential medical readiness resources and refinement in the command and control over wartime support and operation of these resources.8
During contingencies, smoothly running casualty support operations are critical; a lack of joint planning obviously hampers the sharing of limited resources and creates confusion over responsibilities. As the Zimble Report noted in 1984—in a finding that raises problems that might be associated with future sea basing—there was no comprehensive joint plan for the use of the medical assets that were already in place. The services’ contingency medical plans were “stovepipe documents”—that is, their orientations were purely “vertical,” or intraservice—and bore little relationship to each other. This was a direct result of the tendency of the services’ medical components to support their respective line units as if they were the only ones, and likewise a consequence of the lack of a joint medical staff structure to arbitrate differences. There was no mechanism for achieving efficiency through interservice sharing in peacetime, coordinating operations in wartime, or resolving inconsistencies among the components’ plans.9
OPERATIONS DESERT SHIELD AND DESERT STORM
An important element of the medical evacuation process, familiar in both military conflict and civilian mass-casualty disasters, is medical regulation, to which we have already referred. “Medical regulators” manage the process by selecting sources of care, matching patients’ medical requirements with the reported capabilities of treatment facilities. They must also ensure that the receiving medical facilities are not over- or underutilized—an essential matter when numerous and dispersed facilities are involved. During the Persian Gulf War of 1990–91, medical communications problems
represented the greatest limitation in medical regulation, followed by failures of regulating systems to exercise effective oversight of casualty movement. The result was that casualty evacuation was effectively compromised on many occasions.
Communications Problems
Troops on the battlefield could not communicate with ambulances. The radios used by medical regulators had an operating range of only fifteen miles, whereas, for example, the XVIII Corps area was 250 miles deep and a hundred wide. The ambulance units operated with similar equipment and therefore experienced great difficulty in working efficiently with regulators or hospitals. As a result, they often took patients only to hospitals whose locations they knew, and those hospitals were not always the ones best able to assist the wounded. Air ambulances also had difficulty learning where
casualties awaited. One helicopter company, in the words of the General Accounting Office (as the Government Accountability Office was then known), “listened to the international disaster channel to find out where casualties were. . . . After patients were loaded, pilots flew directly
to known hospital locations over Iraqi tanks and infantry. One pilot stated that if it had been a ‘shooting war,’ the company would have lost every Huey [helicopter] and its crew.”10
To overcome these shortcomings of communications equipment, VII and XVIII Corps restricted air ambulances to shuttle runs between designated collection points near the battlefield and drop-off points adjacent to hospitals. As a Navy medical officer with a Marine Corps tank battalion described his situation, “The locations of higher echelon medical facilities were not even available at the battalion or division level.”11
Communications between medical units and between the different levels of care (such as between aeromedical evacuation units and field hospitals) were made even more difficult by the prevailing variety of radio equipment and the use of commercial along with tactical telephone systems. Without adequate communications capability, some Army and Air Force facilities frequently had no warning of the quantity or type of casualties that they were to receive. Some field hospitals did not know that casualties were on the way until the aeromedical evacuation helicopter arrived. Obviously, for them,
planning for patient-care needs was out of the question.12
During the movement into Iraq, some Army hospitals were left for several days with no method of communicating with either combat or evacuation
units. The chief nurse of the Army 12th Evacuation Hospital found its communications in Saudi Arabia nonexistent; the equipment was too diverse and too limited in capability. Helicopters had FM radios with a range of only twenty miles; the field hospitals had AM radios, which in any case could not be used near a battlefield, since their transmissions were traceable by the enemy. Furthermore, while combat and command units had satellite equipment, that did not put them in direct communication with the medical units that lacked such capabilities. Also, due to either traffic saturation or
inherent equipment limitations, none of the systems at aeromedical evacuation locations proved consistently reliable.13
Communications problems for combat and support units, of course, are not new. They were identified during the Urgent Fury invasion of Grenada in 1983, during the 1990 Just Cause contingency in Panama, and during such Joint Staff exercises as Proud Eagle (worldwide), Reforger (Europe), and Team Spirit (Korea).14
Casualty Regulation Breakdown
Communications problems among all services during Desert Shield and Storm degraded the casualty regulating mission. These were primarily related to limitations and mismatched capabilities on both the intra- and inter-service levels. Some medical facilities could not communicate with their control elements, with one another, with supported combat units, or with supporting logistical units.
The inability of medical regulators to manage the evacuation of patients could have led, had the projected numbers of casualties actually occurred, to the underuse of some hospitals and the overwhelming of others—a potentially tragic situation. A “lessons learned” report by the Air Force’s Air Mobility Command stated that as a result of communications problems, 43 percent of patients arrived at the wrong airfield and had to be
rerouted to the appropriate medical facility.
While automated medical regulating systems existed, they were unfortunately not standardized, interoperable, or available in all theatres, and they could not track the location and status of individual patients. Each service had its own computer systems, and the incompatibility of those systems severely limited the ability of medical organizations to interoperate during the war.15
Casualty Evacuation Problems
The process of medical evacuation entails moving patients under medical supervision both to and between medical treatment facilities. The Army and Marine Corps provide most of the ground and helicopter lift for tactical medical evacuation. (The primary Air Force medical mission is to provide fixed-wing aeromedical evacuation within and between theatres.)
In the Persian Gulf conflict, problems arose in the effective use of both ground ambulances and helicopters in tactical evacuation of patients. Ground ambulances could not be used as often as had been planned because of the rugged terrain, a lack of navigational equipment, and the long distances. Even air evacuation was taxed by the distances from pickup points to the hospitals; refuelling was frequently required, and crews had trouble
locating fuel sites. Some air ambulances landed near tanker trucks, tanks, and Bradley fighting vehicles to ask for fuel and for directions to the nearest proper supply.16
Lacking its own tactical medical evacuation assets, the Navy ordinarily relies upon returning (“retrograde”) combat support aircraft with primary missions other than medical. They serve as “transportation of opportunity” for moving casualties to medical facilities afloat and to land-based advanced-echelon medical facilities.
Obviously, because of other priority commitments, such aircraft are not always available in sufficient numbers when urgent medical evacuation requirements arise. In the Gulf in 1990–91, short-range Army and Marine helicopters were available for medical evacuation, but, as Army and Marine Corps officers acknowledged, too few of them—at least in part, as asserted by the Defence Department’s inspector general, because Navy aeromedical requirements had not been previously made known and the Army and Marine Corps had accordingly not arranged to support them. As noted by the Navy’s surgeon general, “lack of dedicated tactical aeromedical evacuation capability in naval services would have created difficulties had the theatre (Southwest Asia) matured as expected.”17
To have had any fewer or less capable Air Force aeromedical evacuation assets would have affected patient care as well. The commanding officer of the Air Force’s theatre aeromedical evacuation squadron later stated that insufficient aircraft were allocated to evacuating patients and that the predicted flow of casualties would have overwhelmed them. Further, even given sufficient aircraft, there were shortages of crews and in-flight evacuation equipment; the Air Force surgeon general was convinced that “we were fortunate that the medical evacuation system was not taxed.” If it
had been, substantial shortfalls in strategic and tactical aeromedical evacuation would have materialized.18
Nobody should have been surprised. Like communications problems, deficiencies in aeromedical evacuation assets are nothing new. They were noted
in several Joint Staff–sponsored exercises, including Reforger in 1987 and Wintex in 1988 and 1989. During the latter, in Europe, a lack of dedicated
aeromedical evacuation assets paralysed the entire combat zone until three thousand exercise casualties could be removed.19
The Air Force, particularly aware before the 1990 Iraqi invasion that it did not possess sufficient personnel or equipment to manage patients needing individualized care during evacuation flights out of Southwest Asia, required that any hospital unit evacuating a patient needing constant attention was to provide an in-flight medical attendant and enough specialized equipment, such as respirators or cardiac monitors, to last five days. Two Navy fleet hospitals were required to provide for additional care at staging sites. These requirements, however, were not taken into account in fleet hospital and hospital ship manpower and equipment authorizations. Had casualty rates approached predicted levels, the inventory of ventilators, intravenous fluids, medications, litters, and a host of other items would have been rapidly exhausted by these evacuation needs.20
In a 1993 report the Defence Department inspector general indicated that operation plans of the commanders in chief still, two years after Desert Shield and Desert Storm, did not promote the efficient use or sharing of medical assets. It indicated that the U.S. Central, European, and Pacific commands did not propose to integrate medical support at all, instead assigning each service component to provide for its own forces only. The report found further that such inconsistencies persisted because of poor testing of medical systems during joint exercises—exercises that included only
token medical participation and could not validate readiness.21
OPERATION IRAQI FREEDOM
Anecdotal reports from surgical staffs, as well as from tactical aeromedical nursing staffs, do not, unfortunately, offer much hope for the future.22 Once again, they related discouraging examples of the state of medical regulation: inadequate coordination/communications between the extraction site and the flight controllers at the Direct Air Support Center–Patient Evacuation Team, as well as between the inbound casualty evacuation aircraft and casualty delivery sites.
Invasion Manoeuvre Phase
The surgical teams related not only difficulty in communicating with evacuation controllers but also that they received no warning of incoming casualties. Likewise, occasional long waits at casualty evacuation pickup points were observed, as well as insufficiencies of personnel or equipment at casualty-drop-off landing zones. The limited communications and limited available airlift likewise made reinforcement or replacement of medical personnel difficult.
Concurrently, training deficiencies of medical personnel were reflected in the relaying of incorrect landing zone coordinates and erroneous patient
priority status, as well as in frequent failure to report to controllers updates in the physical status of casualties prior to pickup. In addition, during the invasion of Baghdad, inexperience and lack of training led to “overtriage” of casualties by frontline medical responders. On the medical evacuation messages, all casualties had been designated as “urgent surgical,” some inappropriately, leading the flight controllers to direct all casualties to the
forward collocated surgical teams, nearly overwhelming their capability. One forward-located surgical team was obligated to care for seventy-eight significantly injured casualties in a forty-hour period, performing surgery upon fourteen in twenty-four hours. Indeed, the combination of communications deficits, lack of available resupply, insufficient return of nurses who had accompanied evacuation flights of casualties, and
physical exhaustion all significantly degraded their capability. As noted at the time by one of the authors, “Only because of an unplanned fifteen hour break, return of the en route care nurses, and serendipitous arrival of supply blocks with commonly used medical consumables, were the teams able to meet another 30 hour period of sustained casualty flow.”23
Transfer of clinical data, including health and treatment status of casualties, from one treatment point to another was not easily accomplished either; charts were sometimes lost or illegible when received at higher levels of care. Attempts were made to convey information by writing on the skin or dressings, but in vain; the notes were often smudged, soaked, or illegible. Nurses assigned to provide en route care attempted to pass on information vital to ongoing care, but time was often limited. (Incomplete information transfer can lead to repeated, and possibly unnecessary, operations.
For example, one combat support hospital backing up the surgical teams re-operated upon every casualty as a matter of policy, mistrusting even the information it had. Another such hospital used a policy of selective re-operation, depending on the information available, the status of the patient, and the perceived experience level of the forward surgeons who had first treated the casualties.) In addition, the forward surgical treatment units, lacking feedback on the outcomes of their interventions, could not know if their practices needed to be changed.
An additional issue consistently seen at this time was that of conflicting perspectives between tactical commanders and medical commanders on the geographic placement of forward medical assets.
Security and Stabilization Phase
During redeployment of Navy medical assets in Iraqi Freedom II,* the location of surgical assets was again often determined by ground combat commanders, who based their decisions upon evacuation times, attempting to ensure that every Marine was within one hour of an operating table, if needed. This once resulted in placement of a Navy FRSS team within twelve minutes’ evacuation time of an established advanced Army combat support hospital, thereby creating redundancy and wasting limited valuable resources that were needed elsewhere, such as during the initial operations in Fallujah.
In May 2004, the Army surgeon general received from his trauma consultant a report regarding theatre trauma care that confirmed many of the above
observations.24 The consultant noted, first, disorganized delivery of trauma care on the battlefield, resulting in nonoptimal staffing and placement of surgical assets, and casualties occasionally being sent to the wrong location. Second, he found, medical records were not reliably reaching the next level with casualties, with a resultant impact upon clinical care and ability to capture aggregate experience.
Finally, he recommended the establishment of a “Joint Theatre Trauma System.” A fully functional joint combat trauma system would embrace all aspects of trauma management, from prevention, training, and evaluation through all phases of care with command and control, as well as data collection, evaluation, research, and process improvement. It would also involve dedicated communications and ensure adequate standards and oversight of first-responder care at the point of injury, initial resuscitative care at the battalion aid station, forward surgery, en route care, definitive care either in the theatre or aboard MPF(F)s or ships of the expeditionary strike group, and finally strategic transportcare beyond the combat zone. The system would be under the oversight of a “corps trauma surgeon,” an experienced trauma physician who would:
Negotiate with ground commanders regarding the optimal locations of facilities with surgical capability
Minimize delays at forward locations and analyse time intervals between different levels of care
Ensure continuous improvement of casualty care at forward levels, on the basis of data accounting for
the great variability of care, outcomes, skills, and circumstances
Optimize evacuation routes Ensure consistent policy regarding en-route interventions by aeromedical nursing staffs
Ensure reliable communications Reduce geographic redundancy between medical
units of various services with similar capabilities Ensure effective communications and logistical
support.
UNANSWERED QUESTIONS FOR SEA-BASE COMANDERS
Recent advances in development of body armour and changing tactical utilization of improvised explosive devices by opposing forces may well have shifted the spectrum of wound survivability. The incidence of mortal wounds of the chest and abdomen may have diminished, thereby allowing greater numbers of casualties with severe injuries to the head, brain, and neck, as well as major blood vessel injuries of the extremities, to survive
long enough to reach forward combat unit medical staffs, such as those of battalion aid stations. Granted, the resuscitation capabilities of battalion medical personnel on the ground, both corpsmen and physicians, are projected to grow. Nonetheless, will the treatment system envisioned under sea basing’s concept of a minimal medical footprint ashore allow timely and competent treatment of these severe injuries?
In 1973, during the Yom Kippur War, a surgical hospital erected by the Israeli Defence Force in the Sinai Desert received casualties in groups of from thirty-six to 140 (on one day 440 casualties), stabilizing them and transferring most to hospitals in central Israel.25 Would not such a volume in a future major conflict quickly overwhelm a limited number of Navy/Marine forward resuscitation and surgical units or equivalent if they were
available in combat service support areas? FRSS units each have only two surgeons, one surgical theatre, a small number of nursing personnel, and no appreciable patientholding capacity. In a sea-base scenario accompanied by a large number of ground combat casualties, would not their inability to sort out types and levels of injuries rapidly, directing personnel needing advanced care to appropriate facilities and returning those with minimal
injuries to their units, result in a mass, hurried, and necessarily indiscriminate transfer of casualties to an offshore medical facility, the sea base itself?
Failure to identify the most needy casualties for evacuation imposes enormous burdens upon transportation assets and afloat facilities. Military
planners unfamiliar with the realities of combat wound management often consider medical evacuation but an exercise in logistics, in which numbers of anticipated casualties, quantifiable capacities of transport facilities, availability times of transport shuttles, and numbers of available beds are the primary considerations. That view ignores the realities of wound care and implies an acceptance of an overall increase in deaths, or at least
disability, and a decrease in the return of men to duty (see photo).
Casualties being evacuated by CH-46, Iraqi Freedom U.S. Navy
How can patients evacuated from a battlefield to a sea-based medical entity be properly routed to the facility best suited to their specific needs? Absent a well practiced and smoothly functioning casualty distribution system, supported by advanced and networked communications, the growing proportion of surviving casualties with severe wounds are likely to find themselves not in the seaborne medical facility best prepared to treat their specific injuries but in the less capable facilities of amphibious assault ships. Ideally, a sea base would include MPF(F) ships with modules capable of advanced neurosurgery to manage brain and spinal cord damage and of vascular surgery to treat complicated blood-vessel injuries. Clearly, time
expended transferring patients with such devastating injuries, without knowledge of their specific needs, from a battalion aid station to a marginally staffed facility aboard an LHD could be fatal, or at least sharply lessen prospects for recovery, and consume limited resources unnecessarily (see figure).
Key:.
APOD air point of debarkation ESG expeditionary strike group
APS Army Prepositioned Stock MPF(F) Maritime Prepositioning Force(Future)
ARF Army Regional Flotilla MPS maritime prepositioning ship
CONUS continental United States SPOD sea point of debarkation
CSG carrier strike group TBD to be determined
Are the necessary medical-regulation capabilities regularly practiced during exercises? In 1994 one of the co-authors was the deputy amphibious task force surgeon in a major Pacific exercise, Tandem Thrust, and in 1997 served as the deputy naval forces surgeon in a combined U.S./Australian Tandem Thrust off the Australian coast. In neither exercise was medical regulation practiced. In fact, actual injured personnel from the afloat task force were flown ashore to a civilian hospital. A report generated by international colleagues who had held medical leadership positions in a later
exercise, RIMPAC 2000, noted a similar lack of medical regulation “play.” Ironically, the report held that the most useful medical communications method in RIMPAC 2000 was unclassified e-mail, which worked throughout the exercise.26
A COMAND MEDICAL ELEMENT
The historical record of dysfunctional medical support during armed conflict reflects persistent neglect of the fundamentals of managing the needs of the sick and wounded. In the setting of joint/combined sea-based operations, dissociated from a land base, therefore, serious consideration should be given to a command entity specifically responsible for operational control over joint medical functions. Such responsibility must be vested in a single entity or individual who is appropriately placed within the command structure, is assigned adequate staff to discharge these responsibilities, and has clearly delineated authority and accountability. Likewise, there must be a clear and functional chain of command within this entity that can develop as well as execute joint medical plans involving the sea base.
This “medical command element” would promulgate local doctrine sufficient to guide not only joint medical planning but also that of each service in the joint task force. Consequently, authority must be delegated by the chain of command to the command medical element to ensure that these principles are incorporated into operational medical planning at every echelon and that the plans developed by service components are both
coherent and compatible.
The medical command element would also:
Ensure that the sea-base medical system can integrate with the joint strategic patient evacuation system in wartime as well as during contingencies.
Ensure that responsibility for control of the tactical and strategic components of the medical evacuation system lies within the same chain of command and that clear guidelines regarding aircraft destinations and patient distributions, as well as priorities for medical evacuation, are promulgated.
Ensure that the system of medical communications at the joint level, as well as within the various components of the sea base, are sufficient to support
wartime medical operations, are simple and direct, and will work reliably during times of crisis. Determine whether the sea base can accept biological,
chemical, or radiological warfare casualties. Ensure that adequate mechanisms exist in the medical planning system for assessing the capabilities of
friendly nations to provide hospitalization and evacuation support in the event of mass casualties, and also for arranging that support via adequate
means of swift communication channels.
Without a well developed medical support plan and methodical testing of its worthiness, the Navy and allied services may not be aware of all the possible impediments to the rapid surge and timely engagement of their forces in response to crises within a sea-base context. A comprehensive set of goals, performance measures, time lines, milestones, benchmarks, and guidance documents are necessary to manage any joint medical response plan effectively and to determine if the plan is capable of achieving its goals. In any case, systematic testing and evaluation in the field of new concepts is an established practice for gaining insight as to how systems and capabilities will perform in actual operations. Commitment to the implementation of these most basic fundamentals of medical support in the field must be firmly established. It is to answer this call that a medical command-and-control entity is proposed. The medical people who are now practicing “good medicine in bad places” are far better prepared than ever before. Now, they need to be given a command structure and proper resources to do their job even better.
Will it work? We must not forget that military innovation and improvements are fostered by developing new concepts and organizational ideas, transferring them into operational reality, and employing them. Table-top and command-post exercises, war games, and experiments have traditionally been applied to these purposes, exploring military doctrine, operational concepts, and organizational arrangements. The concept
of a deployable medical command element is surely worthy of similar consideration.