Introduction
The military demands a high level of physical and psychological health of its members throughout their career. Physical or mental illness may render service members disabled or at least unable to achieve minimum health standards required for their role, at which point they may be discharged from service. Discharge and release from service is an inevitable and necessary part of business. However inappropriate discharge can disrupt future force planning through the number of personnel available for operations, and financially through lost investment and knowledge base. There can also be significant costs associated with the treatment, rehabilitation and compensation of service related medical conditions which are not necessarily recognised and not easily accountable. Although the majority of these costs are covered through New Zealand’s Accident Compensation Corporation (ACC), a number will also receive government funded care in hospital and compensation through New Zealand Veterans’ Affairs. It is therefore of great importance to identify and understand the factors that lead to discharge and to develop appropriate preventive strategies.
Several studies of military populations around the world indicate that initial training is the highest period for discharge from service1-9. These studies also indicate that musculoskeletal related injuries is one of the most common reasons for discharge1,2,5-7,10-12 and is almost always followed closely by mental illness and behavioural disorders 9,13,14. It may be suggested that militaries, and more specifically services, will share similar rates and cause of medical discharge, as most engage in relatively similar activities. However, significant differences exist in
entry standards, risk acceptance, service culture, physical requirements and environmental exposure between and within countries. All of these may play key roles in the development of preventable Service related medical conditions.
There are no reports in the scientific literature regarding the epidemiology of medical discharge in the New Zealand Defence Force (NZDF). The aim of this study was to describe the current epidemiology of medical discharge in the NZDF as a first step towards identifying research priorities for improving medically- related attrition and evidence- based selection standards.
Methods
We conducted a retrospective study reviewing medical files and work force personnel data of all Regular Force NZDF Service members discharged under a medical release category over a six year period between the 1st of January 2006 and the 1st of January 2013. The main source of the data was the NZDF electronic health recording (EHR) system,
which has been operating across the NZDF since late 2005.
For each discharge the reason for medical discharge was determined and coded using the International Classification of Diseases, Tenth Revision, Australian Modification (ICD-10-AM), World Health Organisation, Geneva, Switzerland. Two additional codes in order of importance were used to denote other significant medical conditions that were identified by the reviewing Medical Officer at the time of discharge. These conditions may have contributed to the decision but were not the reason for discharge. The release category (DG1 and DG2) allocated by
medical officers at the time of discharge was also recorded. Service members suffering a condition causing a permanent disability are discharged category DG1, and those who have fallen below an acceptable medical standard are discharged category DG2.
All medical discharges were reviewed to identify if the reason for medical discharge was a result of a condition present prior to entry into the military. Cases were simply grouped ‘yes’, ‘no’ or ‘not known’. Whether the condition was known to the service at the time of recruitment was not explored in this study. Demographic data also collected included gender, age, rank (Officer, Officer Cadet or Enlisted), time in service and service type, Royal New Zealand
Air Force (RNZAF), Royal New Zealand Navy (RNZN) and New Zealand Army (NZ Army). Information on the New Zealand Special Operations Force was not included in this study. Demographic data for the study population were compared with the NZDF population data to generate a prevalence rate per 1,000 individuals. Data were analysed using Microsoft Excel (Microsoft ® Corporation, USA, 2010). The influence of gender on the incidence of discharge across the NZDF was examined and an odds ratio was determined and 95% confidence intervals (CI) were calculated. Two-sample t-tests were used to look at differences in rates by gender. A statistical significant level was set at p <0.05. Ethical approval was obtained in accordance with the NZDF Authority to Conduct Personnel Research, Defence Force Order 21/2002.
Results
Between the 1st of January 2006 and the 1st of January 2013 a total of 7,511 (9.2%) Regular Force Service members left the NZDF, of which 402(0.5%) were discharged for medical reasons. This equated to an annual medical discharge rate of 6.2 per 1,000 with respect to the total NZDF population during this period.
Most service members (88.1%) were medically discharged DG2 for falling below an acceptable medical standard yet there were still a significant number (11.9%) who were discharged DG1 due to permanent disability (Table 1). For the period studied the NZ Army was found to have the highest proportion of discharge through permanent disability (20.5%). Conversely the RNZN had the lowest proportion of discharge for permanent disability (4.2%) yet the
highest overall rate of medical discharge (13.2 per 1,000). This was double that of the NZ Army at 5.32 per 1,000 and significantly higher again from the RNZAF at 1.6 per 1,000. The RNZN annual discharge rate varied between years, in contrast to the other two services where it remained relatively stable (Figure 1).
Mean age ± Standard Deviation [SD] at the time of release was 26.40 ± 7.93 years for NZ Army, 26.22 ± 10.80 RNZAF and 20.89 ± 6.34 years for RNZN. The majority (67.9%) of medical discharges across the services were male (Table 1) and were predominantly represented by younger members (Figure 2). In contrast to this overall trend, within the RNZAF 62% (14/37) of those medically discharged were female. The proportion of female discharges from NZ Army and RNZN were 23.3% and 34.4% respectively.
During the period of analysis females comprised 16.38% of the total Regular Force population. The odds of medical discharge among females compared with males was 2.39, (95% CI: 1.93–2.95), and was statistically significant
(p < 0.0001). Between the year 2006 and 2012 the female to male medical discharge rate ratio was 8.7:3.6 Females were also found to be medically discharged significantly earlier than males. The mean length of service prior to discharge for males was 1478.5 ± 211.0 days and females 870.0 ± 107.8 days and the median length of service for males and female was 806.0 and 321.0 days respectively. There were no significant differences in medical condition however; females were significantly younger at the time of discharge with a mean age ± SD of 22.1 ± 5.4 years in
comparison to males at 24.6 ± 8.9 years (p < 0.004).
Table 1. Demographic characteristics of medical release between services. Cumulative number (n) and percentage (%).
| ARMY (n=176) | RNZAF (n=37) | RNZN (n=189) | TOTAL (n=402) | ||||||
| n | (%) | n | (%) | n | (%) | n | (%) | ||
| Age (years) at time of discharge | |||||||||
| 17-24 | 97.0 | (55.1) | 21.0 | (56.8) | 161.0 | (86.1) | 279.0 | (69.4) | |
| 25-29 | 39.0 | (22.2) | 7.0 | (18.9) | 18.0 | (9.6) | 64.0 | (15.9) | |
| 30-39 | 24.0 | (13.6) | 6.0 | (16.2) | 4.0 | (2.1) | 34.0 | (8.5) | |
| 40 ≥ | 16.0 | (9.1) | 3.0 | (8.1) | 5.0 | (2.7) | 24.0 | (6.0) | |
| Gender | |||||||||
| Male | 135.0 | (76.7) | 14.0 | (37.8) | 124.0 | (65.6) | 273.0 | (67.9) | |
| Female | 41.0 | (23.3) | 23.0 | (62.2) | 65.0 | (34.4) | 129.0 | (32.1) | |
| Release category | |||||||||
| DG1 | 36.0 | (20.5) | 4.0 | (10.8) | 8.0 | (4.2) | 48.0 | (11.9) | |
| DG2 | 140.0 | (79.5) | 33.0 | (89.2) | 181.0 | (95.8) | 354.0 | (88.1) | |
| Time in service (months) | |||||||||
| 0 to 1 | 1.0 | (0.6) | 0.0 | (0.0) | 70.0 | (37.0) | 71.0 | (17.7) | |
| 1 to 2 | 4.0 | (2.3) | 9.0 | (24.3) | 65.0 | (34.4) | 78.0 | (19.4) | |
| 2 to 3 | 1.0 | (0.6) | 5.0 | (13.5) | 4.0 | (2.1) | 10.0 | (2.5) | |
| 3 to 10 | 5.0 | (2.8) | 4.0 | (10.8) | 7.0 | (3.7) | 16.0 | (4.0) | |
| 10 to 20 | 17.0 | (9.7) | 3.0 | (8.1) | 8.0 | (4.2) | 28.0 | (7.0) | |
| 20 to 50 | 59.0 | (33.5) | 3.0 | (8.1) | 9.0 | (4.8) | 71.0 | (17.7) | |
| 50 to 100 | 61.0 | (34.7) | 10.0 | (27.0) | 17.0 | (9.0) | 88.0 | (21.9) | |
| 100 or more | 28.0 | (15.9) | 3.0 | (8.1) | 9.0 | (4.8) | 40.0 | (10.0) | |
| Rank | |||||||||
| Enlisted | 169.0 | (96.0) | 34.0 | (91.9) | 176.0 | (93.1) | 379.0 | (94.3) | |
| Officer | 7.0 | (4.0) | 0.0 | (0.0) | 1.0 | (0.5) | 8.0 | (2.0) | |
| Officer Cadet | 0.0 | (0.0) | 3.0 | (8.1) | 12.0 | (6.3) | 15.0 | (3.7) | |
| Previous condition | |||||||||
| Yes | 16.0 | (9.1) | 9.0 | (24.3) | 36.0 | (19.0) | 61.0 | (15.2) | |
| No | 51.0 | (29.0) | 6.0 | (16.2) | 47.0 | (24.9) | 104.0 | (25.9) | |
| Not known | 109.0 | (61.9) | 22.0 | (59.5) | 106.0 | (56.1) | 237.0 | (59.0) | |
| Discharge each year and as a % of total discharges | |||||||||
| 2006 | 24.0 | (3.4) | 16.0 | (9.9) | 16.0 | (6.4) | 56.0 | (5.0) | |
| 2007 | 26.0 | (3.7) | 3.0 | (1.6) | 34.0 | (11.5) | 63.0 | (5.3) | |
| 2008 | 23.0 | (3.2) | 3.0 | (1.5) | 47.0 | (15.0) | 73.0 | (6.0) | |
| 2009 | 24.0 | (4.9) | 2.0 | (1.7) | 38.0 | (16.5) | 64.0 | (7.6) | |
| 2010 | 27.0 | (5.5) | 4.0 | (3.1) | 9.0 | (6.0) | 40.0 | (5.2) | |
| 2011 | 35.0 | (5.1) | 3.0 | (1.3) | 22.0 | (8.5) | 60.0 | (5.1) | |
| 2012 | 17.0 | (2.3) | 6.0 | (2.7) | 23.0 | (9.0) | 46.0 | (3.8) | |
| Rate of annual medical discharge per 1,000 population | Average | ||||||||
| 2006 | 5.3 | – | 1.4 | – | 8.0 | – | 6.3 | – | |
| 2007 | 5.7 | – | 1.5 | – | 16.7 | – | 7.0 | – | |
| 2008 | 4.8 | – | 1.3 | – | 23.3 | – | 7.9 | – | |
| 2009 | 4.8 | – | 1.9 | – | 18.0 | – | 6.6 | – | |
| 2010 | 5.5 | – | 2.1 | – | 4.2 | – | 4.1 | – | |
| 2011 | 7.2 | – | 2.0 | – | 10.4 | – | 6.3 | – | |
| 2012 | 4.0 | – | 1.0 | – | 12.1 | – | 5.4 | – | |
Figure 1. Rate of medical discharge in NZ Army RNZAF and RNZN between 2006 and 2012 per 1,000
population.
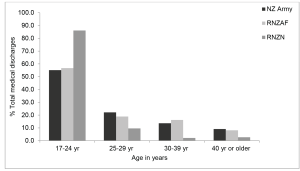
Figure 2. Age at time of medical discharge for NZ Army RNZAF and RNZN (n=402).
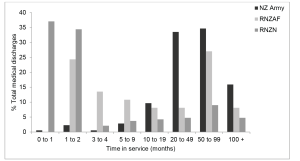
Table 2. Distribution of primary reason for release as percentage by ICD-10 chapter and most frequent individual primary reason for release within ICD-10 chapter. Only individual codes with a rate of ≥ 0.5 percentage of total are included. – no reported cases
| ICD-10 CHAPTER |
% ARMY n=176 |
% RNZAF n =37 |
% RNZN n=189 |
TOTAL COUNT | % OF TOTAL n=402 | ||
| A00–B99 | Certain infectious and parasitic diseases | 0.6 | 5.4 | 1.6 | 6 | 1.5 | |
| B27 | Infectious mononucleosis | – | 5.4 | 0.5 | 3 | 0.7 | |
| B27.9 | Infectious mononucleosis, unspecified | 0.6 | – | 0.5 | 2 | 0.5 | |
| C00–D48 | Neoplasms | 1.7 | 2.7 | 0.0 | 4 | 1.0 | |
| D50–D89 | Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism | 0.0 | 0.0 | 0.5 | 1 | 0.2 | |
| E00–E90 | Endocrine, nutritional and metabolic diseases | 2.3 | 2.7 | 1.6 | 8 | 2.0 | |
| E66.9 | Obesity, unspecified | 1.1 | 2.7 | 3 | 0.7 | ||
| E66.8 | Other obesity | 0.6 | – | 0.5 | 2 | 0.5 | |
| F00–F99 | Mental and behavioural disorders | 27.8 | 29.7 | 10.6 | 80 | 19.9 | |
| F41.2 | Mixed anxiety and depressive disorder | 5.7 | 8.1 | 1.1 | 15 | 3.7 | |
| F32.9 | Depressive episode, unspecified | 5.1 | 2.7 | 1.1 | 12 | 3.0 | |
| F33.9 | Recurrent depressive disorder, unspecified | 1.7 | 2.7 | 1.1 | 6 | 1.5 | |
| F31.9 | Bipolar affective disorder, unspecified | 2.3 | – | 4 | 1.0 | ||
| F07.2 | Postconcussional syndrome | 1.1 | 2.7 | – | 3 | 0.7 | |
| F43.2 | Adjustment disorders | 0.6 | – | 1.1 | 3 | 0.7 | |
| F09 | Unspecified organic or symptomatic mental disorder | 0.6 | – | 0.5 | 2 | 0.5 | |
| F19.1 | Mental and behavioural disorders due to multiple drug use and use of other psychoactive substances, harmful use | – | 2.7 | 0.5 | 2 | 0.5 | |
| F33.2 | Recurrent depressive disorder, current episode severe without psychotic symptoms | 0.6 | – | 0.5 | 2 | 0.5 | |
| F41.0 | Panic disorder [episodic paroxysmal anxiety] | 0.6 | – | 0.5 | 2 | 0.5 | |
| F43.1 | Posttraumatic stress disorder | 1.1 | – | – | 2 | 0.5 | |
| F99 | Mental disorder, not otherwise specified | 0.6 | – | 0.5 | 2 | 0.5 | |
| G00–G99 | Diseases of the nervous system | 5.7 | 5.4 | 2.6 | 17 | 4.2 | |
| G35 | Demyelinating diseases of the central nervous system | 0.6 | – | 0.5 | 2 | 0.5 | |
| G40.3 | Generalised idiopathic epilepsy and epileptic syndromes | 0.6 | – | 0.5 | 2 | 0.5 | |
| H00–H59 | Diseases of the eye and adnexa | – | – | 0.5 | 1 | 0.2 | |
| H60–H95 | Diseases of the ear and mastoid process | – | – | 1.6 | 3 | 0.7 | |
| H83.0 | Labyrinthitis | 1.1 | 2 | 0.5 | |||
| I00–I99 | Diseases of the circulatory system | 3.4 | 0.0 | 3.2 | 12 | 3.0 | |
| I45.6 | Preexcitation syndrome | 0.6 | – | 0.5 | 2 | 0.5 | |
| I47.1 | Supraventricular tachycardia | 0.6 | – | 0.5 | 2 | 0.5 | |
| J00–J99 | Diseases of the respiratory system | 0.0 | 0.0 | 5.3 | 10 | 2.5 | |
| J45.9 | Asthma, unspecified | – | 4.2 | 8 | 2.0 | ||
| K00–K93 | Diseases of the digestive system | 1.7 | 0.0 | 4.2 | 11 | 2.7 | |
| K35.8 | Acute appendicitis | – | 1.1 | 2 | 0.5 | ||
| K50.9 | Crohn’s disease, unspecified | 0.6 | – | 0.5 | 2 | 0.5 | |
| K90.0 | Coeliac disease | 0.6 | – | 0.5 | 2 | 0.5 | |
| L00–L99 | Diseases of the skin and subcutaneous tissue | – | – | 1.1 | 2 | 0.5 | |
| L05.0 | Pilonidal cyst with abscess | – | 1.1 | 2 | 0.5 | ||
| M00–M99 | Diseases of the musculoskeletal system and connective tissue | 38.1 | 29.7 | 28.0 | 131 | 32.6 | |
| M22.2 | Patellofemoral disorders | 3.4 | 2.7 | 3.7 | 14 | 3.5 | |
| M54.5 | Low back pain | 2.8 | 2.7 | 4.2 | 14 | 3.5 | |
| M54.9 | Dorsalgia, unspecified | 3.4 | – | 3.7 | 13 | 3.2 | |
| M23.9 | Internal derangement of knee, unspecified | 0.6 | – | 4.8 | 10 | 2.5 | |
| M24.4 | Recurrent dislocation and subluxation of joint | 1.1 | – | 2.6 | 7 | 1.7 | |
| M15.9 | Polyarthrosis, unspecified | 2.8 | 2.7 | – | 6 | 1.5 | |
| M79.6 | Pain in limb | 1.7 | – | 1.6 | 6 | 1.5 | |
| M86.9 | Osteomyelitis, unspecified | 1.7 | – | 1.6 | 6 | 1.5 | |
| M25.5 | Pain in joint | 2.3 | 2.7 | – | 5 | 1.2 | |
| M51.1 | Lumbar and other intervertebral disc disorders with radiculopathy | 1.1 | – | 0.5 | 3 | 0.7 | |
| M62.2 | Ischemic infarction of muscle | 1.7 | – | – | 3 | 0.7 | |
| M76.5 | Patellar tendinitis | 0.6 | – | 1.1 | 3 | 0.7 | |
| M93.2 | Osteochondritis dissecans | 1.1 | – | 0.5 | 3 | 0.7 | |
| M16.1 | Other primary coxarthrosis | 0.6 | – | 0.5 | 2 | 0.5 | |
| M41.9 | Scoliosis, unspecified | 0.6 | – | 0.5 | 2 | 0.5 | |
| M45 | Spondylopathies | 0.6 | 2.7 | – | 2 | 0.5 | |
| M54.3 | Sciatica | – | – | 1.1 | 2 | 0.5 | |
| N00–N99 | Diseases of the genitourinary system | 0.6 | – | 4.8 | 10 | 2.5 | |
| N93.9 | Abnormal uterine and vaginal bleeding, unspecified | – | 1.1 | 2 | 0.5 | ||
| O00–O99 | Pregnancy, childbirth and the puerperium | – | – | – | – | – | |
| P00–P96 | Certain conditions originating in the perinatal period | – | – | – | – | – | |
| Q00–Q99 | Congenital malformations, deformations and chromosomal abnormalities | 0.0 | – | 0.5 | 1 | 0.2 | |
| R00–R99 | Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified | 2.8 | – | 4.2 | 13 | 3.2 | |
| R69 | Morbidity not stated or unknown | 0.6 | – | 0.5 | 2 | 0.5 | |
| S00–T98 | Injury, poisoning and certain other consequences of external causes | 13.1 | 24.3 | 24.9 | 79 | 19.7 | |
| S82.9 | Fracture of lower leg, unspecified | – | 2.7 | 6.3 | 13 | 3.2 | |
| T79.6 | Traumatic ischemia of muscle | 4.5 | 8.1 | 1.1 | 13 | 3.2 | |
| S93.4 | Sprain and strain of ankle | – | 2.7 | 1.6 | 4 | 1.0 | |
| S09.7 | Multiple injuries of head | 1.7 | – | – | 3 | 0.7 | |
| S82.1 | Fracture of upper end of tibia | – | – | 1.6 | 3 | 0.7 | |
| S82.7 | Multiple fractures of lower leg | 0.6 | – | 1.1 | 3 | 0.7 | |
| S82.8 | Fractures of other parts of lower leg | – | 2.7 | 0.5 | 2 | 0.5 | |
| S83.0 | Dislocation of patella | – | – | 1.1 | 2 | 0.5 | |
| S83.4 | Sprain and strain involving (fibular) (tibial) collateral ligament of knee | – | 2.7 | 0.5 | 2 | 0.5 | |
| S83.5 | Sprain and strain involving (anterior) (posterior) cruciate ligament of knee | 0.6 | – | 0.5 | 2 | 0.5 | |
| S86.0 | Injury of Achilles tendon | – | – | 1.1 | 2 | 0.5 | |
| S92.0 | Fracture of calcaneus | 0.6 | – | 0.5 | 2 | 0.5 | |
| S92.7 | Multiple fractures of foot | – | – | 1.1 | 2 | 0.5 | |
| V01–Y98 | External causes of morbidity and mortality | 2.3 | – | 2.6 | 9 | 2.2 | |
| X60 | Intentional self-harm | 0.6 | – | 2.1 | 5 | 1.2 | |
| Z00–Z99 | Factors influencing health status and contact with health services | – | – | 2.1 | 4 | 1.0 | |
| Z33.1 | Pregnant state, incidental | – | – | 1.6 | 3 | 0.7 | |
| U00–U99 | Codes for special purposes | – | – | – | – | – | |
*Only individual codes with a rate of ≥ 0.5 percentage of total are included. –: no reported cases
The time spent in service before discharge varied considerably between all three services (Figure 3).Thirty seven percent of all RNZN medical discharges occurred within the first month and 71.4% in the first two months of service. Conversely, NZ Army discharged a mere 2.8% in the first 2 months with the majority occurring significantly later in their careers between 20-100 months (Table 1). Close to half (48.6%) of medical discharges from the RNZAF were in the first 10 months of service.There were differences in the rate of discharge between officers vs. enlisted personnel (Table 1). The majority of NZDF members medically discharged were enlisted (94.3%) with far fewer Officer Cadets
(3.7%) and even fewer Officers (2.0%). No Officers were medically discharged from the RNZAF over the duration of analysis.
A number of discharges were found to be a result of pre-existing medical conditions held prior to service (Table 1). The RNZAF discharged 24.3% for pre-existing conditions, while the RNZN discharged 19.1% and NZ Army 9.1%. The most common preexisting condition resulting in subsequent discharge was asthma (9.8%). Of all medical discharges, 72.1% were characterised by three chapters of the ICD-10 coding system (Table 2). The majority were classified within diseases of the musculoskeletal system and connective tissue (32.6%), mental and behavioural disorders
(19.9%) and injury, poisoning and certain other consequences of external causes (19.7%). Within the musculoskeletal system, patello-femoral disorders, internal derangement of knee, fractures of the lower limbs, and back pain were common. The most common mental illness or behavioural disorders reported as reasons for discharge were affective,
anxiety and personality disorders. Discharges having significant co-morbidities allocated as part of their overall reason for discharge accounted for 30.6% of cases. This study chose not to investigate any time course differences in discharge rates of specific chapters or diagnosis.
Discussion
This is the first known published descriptive epidemiological report regarding NZDF medical discharges. The results of this study demonstrate significant variations in the characteristics of medical release between the services. Many studies have shown significant losses early in training 1,6,14 which was true of the RNZN and somewhat of the
RNZAF yet it was in stark contrast to that of the NZ Army. The differences in discharge rates over the years investigated and between the services do not imply a difference in disability rate yet may reflect the local practice of medical management, policy of training units, intensity of training and differences in workplace exposure. The spikes in discharge rates for the RNZN were a result of how medical conditions were managed during initial training at that time. The RNZN tended to formally discharge members from service immediately if they are unable to continue with basic training. If they were to regain medical fitness in the future they would be eligible to reenlist.
This policy was divergent to that of the other services, where members with minor injuries were able to be retained, rehabilitated and re-coursed to the next available intake.
Discharge for health conditions must comply with relevant New Zealand legislation such as the Human Rights Act 1993, which requires employers to take ‘reasonable steps’ to accommodate employees with disabilities. The NZDF can justifiably exclude those who cannot perform the duties required of a service person, or those who would be placed at increased risk to the health of self or others. The results indicate the three services differ in their approaches to accommodating service personnel who are injured or unwell. Although a standard management approach is justified, recruitment and accommodation is highly dependent on the proposed occupation of the
individual and hence individual service capacity to safely manage those individuals may vary. Further studies are recommended to consider differences in medical discharges between trades to identify problem areas.
Females were significantly over represented in medical discharges. Compared to their male equivalents, females were 2.42 times more likely to be discharged for medical reasons; furthermore, they were discharged earlier in their service career and at a younger age. This is consistent with observations of many other studies which show higher rates of injury and discharge from the military in females 4,15-18. The findings present a direct challenge to both Equal Employment Opportunities legislation and Health and Safety legislation. To ensure that the selection and training processes are equitable under Equal Employment Opportunities and Health and Safety legislation, it is recommended that further analysis needs to be conducted to identify the reasons for, and the factors that lead to, increased medical discharges among female service members within the NZDF.
This study identified that at least 15.2% of NZDF personnel were discharged as a result of pre-existing medical conditions. Health screening is an important aspect of the military recruitment process. Although medical and psychological screening processes attempt to identify individuals with significant predispositions or active health problems, there are instances where individuals can pass through the system undetected. It is not known if these discharges were a failure of the applicant to disclose pertinent information or deficiencies with the medical screening
process. In either case, unsuitable enlistment can have negative consequences for the member and the service. This includes increased risk of injury or harm to the individual – for the service there is an increased risk of harm to others, reduced individual or unit performance and potentially increased costs associated with their treatment and management. Notwithstanding the inherent limitations in the collection and interpretation of this data, it does
indicate the need for further investigation. Continued surveillance and reporting of medical discharge data should in part provide important information for the validation of current screening systems to improve medical recruiting standards.
The prevalence of mental health conditions in the NZDF population is unknown. The level may be different to that of the general population due to initial screening and training that may create a healthy worker effect 15. It is accepted that some mental health conditions may develop in military personnel confronted with considerable occupational
stress through combat and day to day operations 16. Yet there is a significant number of mental health conditions that do not develop as a result of combat or deployment exposure. A significant proportion of medical discharges in this study were a result of mental illness and behavioural disorders. The most commonly reported were affective and anxiety disorders and disorders of personality. It should be noted that a disorder of personality would be preexisting
condition, but was diagnosed during service.
This finding supports other studies that have shown mental illness to be one of the leading causes of morbidity in the military9,13,14,19. Further analysis of mental health discharge data is required regarding specific areas of concern rather than a statistic of common mental health codes. Although differences in classifications and methodologies of other studies make it difficult to compare overall discharge rates, the NZDF rates do appear higher than the Australian Defence Force at 10-15%20 and that of the Royal Navy at 8%21.
Discharge rates do not provide an appreciation of the true burden of mental health. It is not known how many of those who seek or are directed to medical support for a mental health condition are subsequently discharged. Multiple avenues for mental health support do exist in the NZDF which include Medical Officers, Psychologists and
Chaplains. However, significant barriers exist in the military due to stigmatisation of mental illness and the seeking of care22-24. Seeking care for mental health is often perceived as a sign of weakness and many are sceptical that mental health services can remain confidential to those who are required to know 23. Gould et al22 and Warner et al24 both demonstrated that scepticism in military personnel more often arose from their concern of how they would be treated by peers and most importantly by their own leadership. A recent study by Rand25 showed that 20% of
military service members returning from Iraq and Afghanistan reported symptoms of post-traumatic stress disorder or major depression, yet only about half have sought treatment. Considering that stigma exists and perceived barriers are similar to other national military services including the NZDF 22,26, one must question how many personnel are not seeking or getting the medical support they require. Analysis of the mental illness and behavioural
discharges against current entry medical screening processes and policy is recommended. Further analysis is also required to investigate the aetiology and epidemiology of mental illness and behavioural disorders in the NZDF along with an examination of the barriers to receiving mental health care in day to day operations at home and overseas.
Musculoskeletal injury and disease is well recognised to be a leading cause of morbidity in most military populations5. Musculoskeletal injuries, especially to the lower limbs, are known to contribute significant
morbidity in the NZDF27 and unsurprisingly form part of the leading cause of medical discharge as described here. The majority of injuries are known to result from individual or team physical training and sports and not operational activities or military training27. However, the true burden of musculoskeletal injury and disease may not be
reflected by the service discharge rates because of differences in their medical management and training policies. Further examination of the data is recommended to investigate areas of commonality between musculoskeletal morbidity codes across ICD-10 chapters.
It must be acknowledged that this study is not exhaustive of the aetiology and epidemiology of NZDF medical discharge. However, it does provide a preliminary investigation into the demographics of personnel and prevalence of conditions among the services. It also provides a rationale for future research into preventative approaches for the health and wellbeing of NZDF personnel.
There are some limitations to this report. Firstly, it is important to highlight the possible inaccuracy of the data entered into the EHR and how personnel were managed. Despite there being some processes in place to ensure that there is standardisation of reporting and management, not all cases were managed equally, an example being that some cases were “medicalised” when they should have been administratively discharged and vice versa. Local practice, a lack of policy and the seniority of staff may all contribute to how cases are managed within the NZDF. Therefore it is important that this error is considered when interpreting the results of this study. Secondly, the study was unable to link clinically important co-morbidities, relationships and areas of commonality beyond ICD-10 chapters. Some of the terms and phrases used to refer to a reason for discharge were in fact synonyms of the same concept. Misclassification bias can therefore result where poorly defined descriptions for medical release are given. Further research is required to investigate mapping epidemiological data like this from strict mono-hierarchy taxonomy like ICD-1028 to poly-hierarchical systems like SNOMED CT29 that may reveal richer relationships of common codes.
The NZDF has a challenge to recruit the right people with the right skills to meet both force element and business roles. In order to do this they must ensure that scientifically reliable and valid physical training and medical standards exist to meet these requirements and relevance to current and future military operations. A balance is required to optimise health-related operational capability by maximising the recruiting pool without impairing operational capability through preventable morbidity, mortality and unnecessary costs. Health practitioners and
personnel managers must work together in order to enhance force preparation and sustainment through
evidence -based advice. Innovative surveillance and meaningful reporting of health data such as this is crucial to validate health initiatives and provide a policy that seeks to train and sustain a force economically.


