R. Linwood, N. Duff, A. Stewart, Flint, M. Reade, P. Krohn, A. Williams, B. McCall
Abstract
Improvements in clinical governance in Australian Army health services in recent years have reflected and drawn upon developments in the civilian sector. This paper describes how 2 GHB adapted and incorporated key civilian health system measures to drive improvements in the quality and safety of clinical care. Health restructure initiatives included optimisation of corporate and clinical governance by introducing a Director of
Clinical Services to assist the Commanding Officer, a similar structure for technical and command authority to that found in modern civilian hospitals. A Clinical Governance Framework was introduced to provide a platform for identifying and addressing areas for improvement, acknowledging that the delivery of health care endeavours to meet the expectations inherent in the Australian standards while taking place in a unique and often austere environment with no readily comparable Australian civilian benchmark. The framework included a dedicated process to evaluate and improve clinical services based on the National Standards promulgated by the Australian Commission for Safety and Quality in Health Care with a view to achieve external certification of a deployable R2E capability. Clinical governance measures were intensified in 2015 as part of preparations for the deployment of a R2E to Operation OKRA, Australia’s support to Iraq in combating Da’esh. These measures included intensive, realistic clinical training and collective certification exercises (HOSPEX) evaluated by expert independent assessors. During Operation OKRA the Clinical Governance Framework was tailored to meet the challenges of health care in a specific operational setting. All authors declare no conflict of interest.
Introduction
The delivery of health care in the deployed military environment has many challenges. These include the complex and labile requirements of the supported force, the austere, potentially hostile environment and the limited availability of health personnel, equipment and resupply that would be regarded as ‘the norm’ in civilian settings. In Australian health care, especially in the last decade, there have been emphatic changes in regulations, structures and processes to deliver health care of a standard that meets community expectations and which embraces safety and quality at its very core. These developments in ‘clinical governance’ have included improvements in the registration and credentialing of health practitioners, requirements for continuing professional development, and adoption of national standards to drive improvements in specific aspects of the quality and safety of health care1.
Australia’s military lead in the provision of deployable surgical capability (NATO Role 2E or R2E) is the 2nd General Health Battalion (2GHB). As
a deployable hospital, 2GHB has unique challenges in maintaining the preparedness of its clinical workforce, equipment and procedures. It addresses
these challenges through a number of measures including partnerships with civilian hospitals (for clinical experience and benchmarking of processes)
and the involvement of Army Reserve health specialists in supporting alignment with civilian practice developments and standards.
In 2010 the CO of 2GHB recognised the important impact that a strong clinical governance framework could contribute to the delivery of safe, high quality health care, particularly within the limitations of the deployed environment. Since then 2GHB has drawn upon civilian experience in clinical governance to develop and implement a series of initiatives to support and strengthen clinical governance in a deployed military setting. Key measures included:
• development of a CO Directive on Clinical Governance;
• introduction of a Clinical Governance Framework (CGF) supported by the creation of a Directorate of Clinical Services to provide leadership and
oversight of the quality improvement processes;
• incorporation of the ten national ACQSHC standards mandated for civilian hospitals2; and
• adoption of the UK Hospital Exercise (HOSPEX) as a means of ‘certifying’ the ability of 2GHB to meet and provide a suitable standard of health
care3.
The impact of these initiatives was validated when 2GHB was tasked in 2015 to support Operation OKRA, a deployment to the Middle East Area of
Operations (MEAO). This paper describes the experiences of 2GHB in terms of the Army Combat Health Restructure, development of a CGF, force
preparation and clinical governance on deployment in Iraq.
IMAGE CAN BE VIEWED IN FULL DOWNLOAD
Image 1: 2 GHB deployed in the field in 2014
Army Combat Health Restructure
Prior to 2010, 2GHB had functioned under the sole direction of its CO. The CO had responsibility for all aspects of the unit’s field hospital service delivery, including clinical output, administration, defence and survivability in the field. Civilian hospitals have addressed the problem of leadership overload by creating a management diarchy – a Chief Executive Officer focussing on general management, and a Chief Medical Officer for clinical matters. The Chief Medical Officer is responsible for all clinical matters including the technical supervision of healthcare staff.
In 2010 as part of the Army Combat Health Restructure, the decision was taken to mirror civilian practice by separating the command leadership
and management function from that of clinical leadership. Accordingly, the position of Director of Clinical Services (DCS) was created at the Colonel
level to attract and exert the appropriate level of clinical and military experience. As the most eligible candidates for the role were Reservists (specialist clinicians in civilian employment), it was decided to supplement this appointment with the Regular Army Senior Nursing Officer appointed as the Deputy Director Clinical Service (DDCS) at the Lieutenant Colonel level. The DDCS was given responsibility for workforce training, particularly focussed on unit nurses and medics, while the Senior Medical Officer (SMO) retained oversight of the development of the unit’s Regular Army General Duties Medical Officers.
This arrangement had two distinct advantages in addition to separating the responsibility for general management from clinical service delivery. The
partnership (combination) of medical and nursing leadership led to mutual understanding of patient needs across the continuum of patient care, vital to managing any hospital workforce. Secondly, with one incumbent a Reservist and the other a Regular officer, continuity of work output and coordination when the unit is not deployed was enhanced. In the field on exercise, the working relationship strengthened, and the capacity for continual technical supervision of healthcare safety and quality assured.
Access to health Reservists brought significant civilian expertise and corporate knowledge. This substantial “value-adding” created access to clinical and general management tools that 2GHB might otherwise have had to develop. Examples included a Clinical Risk Register already attuned to international standards (ISO 31000), and knowledge of casemix data for evidence-based training simulations.
Along with this key change in corporate and clinical governance management came the rationalisation of sub-units specialising in the clinical and clinical support functions necessary for an autonomous field hospital. A departmental focus and culture was achieved, with military groupings broadly replicating civilian hospitals. It is now common to hear unit members speak of being “OTs or Theatre Techs” (Operating Theatre Technicians) rather than Nurse Assistants posted to the Surgical Company.
The DCS/DDCS combination took responsibility for several support functions and processes to enhance patient care. These included clinical skills
training for individuals and teams, monitoring current and upstream medical developments, and the maintenance of credentialing for posted
and contracted clinical staff. Across the unit, communication structures were improved to ensure the best possible consultation and co-operation
occurred to supplement the corporate governance (or command) function inherent in all complex organisations. Corporate communications such as
Standing Operating Procedures (SOP) were reviewed to ensure clinical needs were accommodated, with SOPs specific to the clinical function modernised and benchmarked with civilian practice.
Development of a Clinical Governance Framework and certification of a deployable R2E capability
The adoption of a formal framework for clinical governance has been essential to improving safety and quality in health care provision at 2GHB.
A clinical governance committee chaired by the DCS and inclusive of the CO, heads of clinical Departments and professional leads (e.g. SMO, SNO,
Training, Infection Control and Patient Safety Officer) met regularly to focus initially on improvements in clinical education and training, clinical audit, clinical effectiveness, transparent clinical practice review, risk management and research. This forum paralleled the unit’s existing command conferences chaired by the CO, with significant dual membership enhancing cross-communication. Informing and collaborating with higher formation processes strengthened the CGF and formally incorporated Continuous Quality Improvement (CQI) processes, committing 2GHB to benchmark its standards and processes against Australian civilian healthcare providers using the same CQI tools and measures.
From 1 January 2013, all Australian civilian hospitals and clinical day care facilities were required to adopt new safety and quality standards. Developments over the preceding years led to the National Reform Agenda for the provision of healthcare in Australia. That Agenda includes the derivation of universal National Quality and Safety in Health Service (NQSHS) Standards. These Standards are determined by the Australian Commission for Quality and Safety in Healthcare (ACSQHC), represent agreed best practice and are now mandated under legislation for all healthcare providers operating under the jurisdiction of the states and territories.
The Standards comprise:
1. Governance for Safety and Quality in Health Service Organisations
2. Partnering with Consumers
3. Preventing and Controlling Healthcare Associated Infections
4. Medication Safety
5. Patient Identification and Procedure Matching
6. Clinical Handover
7. Blood and Blood Products
8. Preventing and Managing Pressure Injuries
9. Recognising and Responding to Clinical Deterioration in Acute Health Care
10. Preventing Falls and Harm from Falls
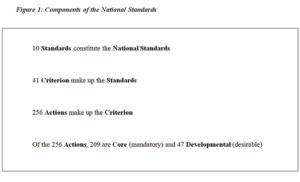
Each of the Standards consists of several Criteria, and Actions to support each of the Criterion as shown in Figure 1. Standards are subject to revision,
validation and update, the next iteration scheduled for 2017. The Standards will form the basis for service provision and comparative benchmarking for the foreseeable future.
Legislation does not mandate NQSHS standards compliance by Commonwealth (e.g. Defence) health providers. However, 2GHB chose to adopt the
National Standards approach to support CQI within the Unit because it clearly aligned 2GHB to national (community) expectations for patient safety and quality and it formed a framework for any future accreditation/certification of health services (1).
In 2013, a dedicated CQI project commenced with the engagement of a specialist CQI coordinator to ensure high level input and project continuity. The project team was formed with the designation of a Standard Leader and a backup member for each of the ten National Standards to ‘insure’ against changes to personnel through posting or deployment. Training and briefings were conducted to incorporate the necessary process and content knowledge.
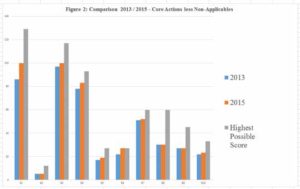
The project began with a self-assessment and gap analysis against all 209 Core Actions (as described in Figure 1). Some of the remaining 47 Developmental Actions were included. The self-assessment yielded a rich quantum of evidence about what was already in place, and what was not. The gap analysis commenced in 2013, led by the Standard Leaders with the support of the project coordinator. Each Standard team came together periodically for peer review, analysis and collective consensus on the “organisational health” of 2 GHB. This step resulted in the identification of key areas including patient identification and documentation, infection control and clinical handover. This led to a formal Action Plan for implementing improvements (e.g. SOP). Some actions were readily amenable to improvement, others required significant investment. The outcome of the Action Plan and the measure of improvement in the self assessment between 2013 and 2015 is described for each Standard (S) in Figure 2. A score
for each Core Action was assigned as Significant work required: 1, Progress made: 2, Met :3, with the highest possible score (HPS) being a 3 in every Core (mandatory) Action.
The final step in the CQI project plan is the accreditation process. While not yet mandated for the ADF, accreditation by independent authorities such
as the Australian Council on Healthcare Standards provides external oversight and reassurance that 2GHB will meet the expectations of the community in the delivery of safe, high quality clinical care.
Force preparation
The preparation for deployment to support operations or exercises fully occupies 2GHB. If the unit is not deployed on exercise or operations, it is
preparing to do so. Preparation and training occurs at an individual, team, sub-unit and unit level on a continuous cycle.
Credentialing of all health practitioners at 2GHB is the first step in ensuring a suitably trained health workforce. 2GHB introduced credentialing
procedures consistent with civilian best practice and has contributed to further developments on this topic within the wider ADF. It also utilises the
credentialing process to identify individual training requirements to ensure suitably trained and capable staff are supported in their role.
Within barracks individual clinical skills are maintained through a series of placements with civilian hospitals and ambulance services. These
placements support the retention and development of skills through exposure to a wide range of clinical settings, working alongside and under the supervision of specialist clinicians (often Reservists). It also exposes clinicians to current practice, providing necessary continuing professional development. In return, many are able to impart their own clinical experience to the benefit of the civilian agency.
Substantial clinical preparation (of individuals and teams) adds to the requirement for generic military skills and fitness required of Army. High fidelity clinical training, with a policy of minimal notionality, is central to this preparation, with cases drawn from trauma registry data of injury from recent and current operations. Training is conducted in the context of known and likely deployments and as realistically as possible.
IMAGE CAN BE VIEWED IN FULL DOWNLOAD
Image 2: Medics in a simulated casualty handling scenario
The Army Training continuum provides for individual, team and sub-unit preparation that culminates in larger full scale exercises to bring together all the elements of the R2E to practice against the full gamut of possible clinical scenarios. The Primary Survey Exercise series provides a two
phase approach of consolidation of clinical training (Phase 1) and collective training for the entire R2E against scenarios which test the process from point of injury to definitive care (Phase 2). These exercises allow the complex interactions of the hospital and its sub-functions to be exercised altogether. It is through this collective exercising and testing that 2GHB identifies improvements and seeks its 2RE capability certification.
Certification exercises are the final step in ensuring that the deployed R2E is ready. Since 2013, 2GHB has expanded the previous hospital certification process to conform to the UK HOSPEX model (3). The strength of HOSPEX is in the use of independent current subject matter experts to formally assess the performance of the R2E against predetermined performance indicators strongly correlated to the mission requirements and in a range of testing clinical scenarios.
IMAGE CAN BE VIEWED IN FULL DOWNLOAD
Image 3: Practising and assessing the continuum of care are vital to CQI, focusing on “no blame” and full disclosure
Clinical Governance during deployment on Operation OKRA
The conventional land force training component of Operation OKRA, the Australian Government’s assistance to the Government of Iraq in combating
Islamic State/Da’esh, commenced in May 2015. The main focus of the 400-strong Australian and New Zealand land force contribution was to provide
training for Iraqi Army infantry brigades rotating through the Taji Military Complex. Coalition health assists in Iraq in 2015 were scarce, and weather
(particularly dust) precluded aeromedical retrieval on many days. The combined ADF/NZDF Task Group consequently deployed with an ‘ANZAC’ Role 2E hospital, the only surgical capability within the Taji Military Complex.
Operational and governance procedures implemented at the ANZAC Role 2E hospital closely mirrored those developed by 2GHB. The OC (a health
General Service Officer) and the DCS each possessed extensive and appropriate experience for their roles. The OC took responsibility for personnel leadership and management, liaison, infrastructure and resupply. The DCS was the technical representative of the Surgeon-General ADF in ensuring the optimal clinical functioning of the hospital within the capability provided by the OC. Based on the 2GHB CGF, a Clinical Governance Directive was tailored to a range of locally-relevant applications, including provision for reporting, audit and patient feedback, haemovigilence and infection control reporting. In virtually every area of hospital practice, by its own assessment and that of the Task Force senior health officer (J07), the ANZAC Role 2E hospital met or exceeded Australian civilian hospital standards.
Specific tasks undertaken in the establishment phase of the hospital were classified according to the 10 ACSQHC Standards:
• Standard 1: Establishing a committee structure that gave clinicians ownership of the CQI process, including weekly morbidity / mortality and
equipment resupply conferences and monthly haemovigilance and infection control committee meetings. These subcommittees reported to
the weekly clinical governance meeting, which reported to both the command and technical control chains to the Commander Joint Operations and SGADF.
• Standard 2: A Patient Safety Officer was appointed, and patient feedback process instituted.
• Standard 3: An outbreak of severe gastroenteritis provided the opportunity for a primary carebased epidemiological investigation and infection
control audit, with several important infection control measures implemented that resulted in the prompt termination of the epidemic.
• Standard 4: A list of nurse / medic initiated medications was approved; a 20% random documentation audit was commenced, with
results fed back through the CG committee to individual practitioners.
• Standard 5: A new SOP was written for ‘patient admission’ that included patient identification policy.
• Standard 6: Formal ward rounds commenced; Identify, Situation, Background, Assessment and Recommendation (ISBAR) training provided and
this process was enforced in morning / evening nursing reports.
• Standard 7: A massive transfusion protocol and emergency (without crossmatch) transfusion protocol was established. An audit of likely
blood use and wastage rates was submitted to the US Armed Forces Blood Program, with one consequence being the establishment of an
Emergency Donor Panel for the provision of whole blood.
• Standard 8: A pressure injury reduction strategy was incorporated into the new admission SOP.
• Standard 9: The deteriorating patient / code blue SOPs were revised to match local environment, personnel constraints, and the physical layout
of the hospital. Ward charts were changed to a ‘between the flags’ format with a request made to modify the official ADF form.
• Standard 10: Modifications to certain parts of the hospital were made to reduce the falls risk. A falls assessment tool was introduced as part of
the admission SOP.
The CG committee spent much of the first three months addressing issues with deployed equipment. The authority to accept clinical risk of certain levels was defined in the SGADF-approved CG Directive, with almost all able to be tolerated or mitigated by the DCS at the local level without the need to refer to remote governance authorities. Clear definition of the authority of the DCS to accept or not accept risk was invaluable in rapid generation of the R2E capability.
Two issues for improvement were almost immediately identified:
• Standard 1: The lack of utility of Army Health Instructions in the deployed Joint or International environment. This required development of
local policies to support clinical practice in a workforce that included RAN, RAAF and Coalition practitioners.
• Standard 4: The use of 2GHB forms (e.g. vital signs charts) that were introduced as improvements to officially endorsed ADF forms was problematic
in the Joint operational environment. Changes recommended in barracks must be promptly incorporated into ADF documents.
The “command philosophy” of the DCS was to treat identification of any deficiencies as opportunities for improvement and as markers of success of the clinical governance system, thus consistent with a CQI approach. This may be at odds with the notion of an immediately deployable, universally
competent and capable organisation. However, it highlights the critical importance of a technical as well as operational reporting chain and justifies the faith and the investment in clinical governance that commenced at 2GHB in 2010.
Conclusion
The success of the first operational deployment of an Australian R2E hospital in ten years was enhanced through the process of clinical governance that had been underway at 2GHB. In the last five years 2GHB has embraced clinical governance, implementing a framework of structural and procedural reform, audit and review that allowed all members to be involved in decision making to support clinical safety and quality and which culminated in the R2E deployment to Operation OKRA. However, the ‘continuous’ nature of CQI means that further effort and improvements will always be required.






