Analgesic use in Vietnam Veterans’ with Musculoskeletal Pain
Lisa Kalisch Ellett, Nicole Pratt, Elizabeth Roughead
Abstract
Background: International studies suggest that high-dose opioid use is more common in veterans with post-traumatic stress disorder (PTSD) than those without in the treatment of musculoskeletal pain.
Purpose: This article aims to examine the use of analgesics by Australian veterans with musculoskeletal pain by conducting a drug utilisation evaluation and to examine use by PTSD status.
Methods: A cross-sectional study of Vietnam veterans with musculoskeletal pain was conducted using Australian Government Department of Veterans’ Affairs (DVA) data. The study reviewed the proportion of dispensed prescription analgesics between 1 July 2015 and 30 June 2016.The volume of opioids dispensed per veteran was calculated as oral morphine equivalents (OME). Results were stratified by PTSD status.
Results: 10 318 Vietnam veterans with musculoskeletal pain were included and 59% were dispensed analgesics. The most frequently dispensed analgesics were paracetamol (dispensed to 31% of veterans with PTSD and 28% without PTSD; p<0.01) and paracetamol with 30 mg codeine (19% of veterans with PTSD and 16% without; p<0.0001).Opioid analgesics were more likely to be dispensed to veterans with PTSD than without (35% v 32%, p=0.002); however, there was no significant difference in the volume dispensed (median of 1.2 [interquartile range (IQR) 0.4–5.8] OMEs per veteran per day for those with PTSD, compared to median 1.3 OMEs [IQR 0.4–6.3] per veteran per day for those without, p=0.3).
Conclusion: Many veterans with service-related musculoskeletal pain did not receive prescription analgesics. Veterans’ with PTSD were more likely to be dispensed analgesics than those without, but PTSD did not appear to influence the volume of opioid dispensed.
Key words: musculoskeletal pain, Vietnam veteran, opioid, analgesic, post-traumatic stress disorder
Introduction
Musculoskeletal pain is common. Systematic reviews of studies published worldwide between 1980 and 2009 for the Global Burden of Disease 2010 study found that the age-standardised point prevalence of lower back pain was 9.4%, neck pain was 4.9%, osteoarthritis was 3.8% and other musculoskeletal disorders was 8.4%.1 Prevalence of lower back pain was highest in men, while all other types of musculoskeletal pain prevalence was highest in women. Prevalence increased with age, although the ages of peak prevalence varied by pain type (e.g.prevalence of neck pain was highest at age 45, while lower back pain prevalence was highest at age 80).1 Within Australia, 22% of men and 27% of Australian women have a musculoskeletal condition, and prevalence increases with age: more than half of men and more than two-thirds of women aged 65 or over report having a musculoskeletal condition.2
Musculoskeletal pain is also common in veterans. Musculoskeletal problems are the most common comorbidity treated at US veterans’ health administration facilities for veterans who served in Operation Enduring Freedom (OEF) or Operation Iraqi Freedom (OIF).3 A survey of British veterans who served in the Gulf War (n=2735), Bosnia (n=2393) or who served in the armed forces but were not deployed to either of these conflicts (n=2422), found that the prevalence of back problems was 36%, 24% and 28% in each of these cohorts respectively.4 Musculoskeletal pain is also common in older veterans. A 2006 report from Australia involving veterans who most commonly served in World War II or the Vietnam war, and their spouses, found that 47% reported having back pain and 51% reported having osteoarthritis or rheumatoid arthritis.5
Musculoskeletal pain can be managed with non-pharmacological strategies; however, in some cases analgesics are required.6 Paracetamol or non-steroidal anti-inflammatory drugs (NSAIDs) are recommended for mild pain and opioid analgesics should be reserved for severe pain.7 Opioid analgesics should only be used short-term for musculoskeletal pain as there is limited evidence to support long-term use.7 In addition, only one-third of patients will benefit from opioid analgesics for musculoskeletal pain and for those who receive a benefit, maximal pain reduction is 50%, while eight in ten will report an adverse event.6
Although several studies have examined the use of opioid analgesics in the general Australian population, none have specifically examined opioid analgesic use among Australian veterans. International studies have shown that use of opioid analgesics for pain management is higher in veterans with post-traumatic stress disorder (PTSD) compared to those without PTSD and that high-risk use is more common in those with PTSD.8 A study involving 141 029 US veterans who served in Afghanistan or Iraq who had non-cancer pain found that 15 676 (11%) were dispensed opioids to manage the pain.8 Compared to veterans without any mental health disorder, those with PTSD were more likely to use opioids at high dose (adjusted relative risk (RR) 1.42, 95% CI 1.31–1.54), were more likely to use opioids long-term (RR 1.47, 95% CI 1.42–1.53), were more likely to use more than one opioid analgesic at the same time (RR 1.87, 95% CI 1.70–2.06), were more likely to use sedative or hypnotic drugs at the same time as the opioid analgesic (RR 5.46, 95% CI 4.91–6.07) and were more likely to have their opioid prescription re-dispensed more than one week earlier than the expected end date of their prescription (RR 1.64, 95% CI 1.53–1.75).8
International studies show a high prevalence of musculoskeletal pain among veterans with PTSD and that problematic use of opioid analgesics may be more common among veterans with pain and co-morbid PTSD. However, there are no published studies on the use of analgesics for chronic musculoskeletal pain in Australian veterans or the influence of PTSD status on analgesic use. Extrapolation of results from international studies may not be relevant to the Australian veteran population due to differences in age and gender, with the Australian veteran population comprising of more men and older age groups than international veteran cohorts. Additionally, differences in access to medicines and the types of analgesics available between different countries limit the usefulness of extrapolated results from international studies. Therefore, the aim of this study was to conduct a drug utilisation evaluation of analgesics by Australian veterans with musculoskeletal pain and examine use by PTSD status.
Methods
Data for this study were sourced from DVA’s administrative claims database. The DVA administrative claims database contains details of all prescription medicines, medical and allied health services, and hospitalisations provided to veterans for which DVA pay a subsidy. The data file contains records for a current treatment population of 200 000 members of the veteran community. DVA maintain a client file, which includes data on gender, date of birth, date of death and family status. Medicines are coded in the dataset according to the World Health Organization (WHO) Anatomical Therapeutic Chemical (ATC) classification system9 and the Schedule of Pharmaceutical Benefits item codes.10 Hospitalisations are coded according to the WHO International Classification of Diseases (10th Edition), Australian Modification.11
Vietnam veterans were included in the study if they were alive on 30 June 2016 and had an accepted service-related disability for chronic musculoskeletal back or knee pain, effective before 1 July 2015.For these veterans we identified analgesic use between 1 July 2015 and 30 June 2016.Analgesics were defined as paracetamol (ATC code N02BE01), paracetamol in combination with codeine (ATC code N02BE51), opioid analgesics (ATC code N02A) and NSAIDs (ATC code M01A).PTSD was identified if a Vietnam veteran had a record in the disability file for service-related PTSD and where the disability was accepted as service related before 1 July 2015.
We identified the number of Vietnam veterans with a service-related musculoskeletal pain disability who were dispensed each type of analgesic. Demographics of study participants were identified, including age at 1 July 2015, gender, type of residence at 1 July 2015 (community or residential aged care), remoteness of residence at 1 July 2015 (major city, inner regional area, outer regional area, remote area or very remote area based on the Australian Standard Geographic Classification) and socioeconomic status based on postcode of residence at 1 July 2015 (using socioeconomic indexes for areas [SEIFA]).Results were stratified by PTSD status. Chi-squared tests were conducted to determine differences in the percentage of Vietnam veterans with and without PTSD dispensed each type of analgesic.
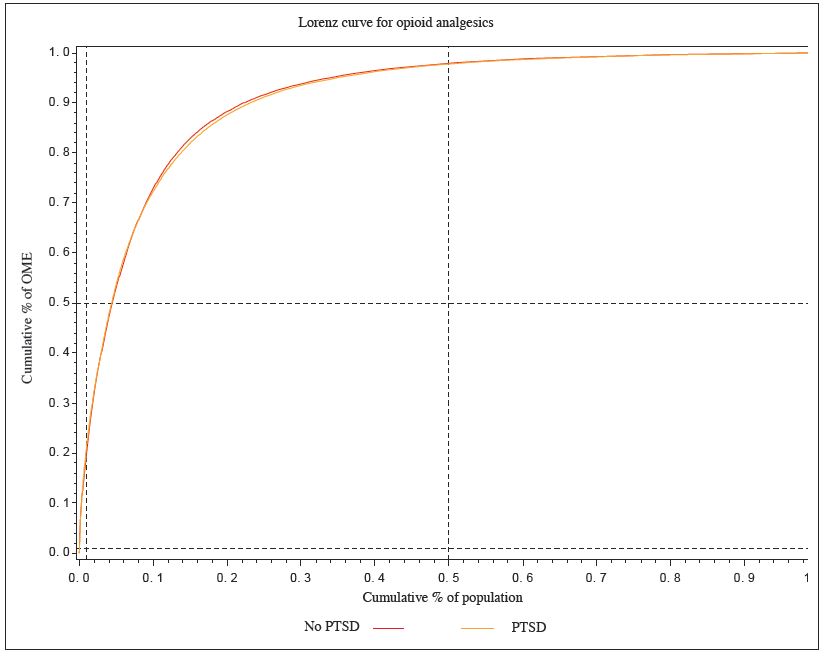
To provide an estimate of the volume of opioid analgesic use over the 1 year study period, the volume of opioids dispensed to study participants was calculated as ‘oral morphine equivalents’ per veteran per day, using the conversion table developed by the Australian National Drug and Alcohol Research Centre.12 We calculated the oral morphine equivalents (OME) supplied at each opioid dispensing by multiplying the OME conversion factor for each opioid by the mass of analgesic in each tablet and the number of tablets supplied at the dispensing. For example, oxycodone has an OME conversion factor of 1.5, so a dispensing of 20 oxycodone 5 mg tablets contains 1.5×20×5 = 150 OMEs, equivalent to 150 mg of morphine. The total OME for each opioid analgesic dispensed to each veteran over the year was calculated, then divided by the number of days in the year (365) to provide the average OME per veteran per day. Differences in the median OME per day were compared for veterans with and without PTSD using the Wilcoxon test. We also expressed the cumulative percentage of opioid OMEs dispensed, by the cumulative percentage of patients using opioids, stratified by those with and without PTSD as a Lorenz curve.13 All analyses were performed using SAS for Windows, V9.4 (SAS Institute, Cary, North Carolina, USA).Approval to conduct the research was obtained from the University of South Australia Human Research Ethics Committee and the Department of Veterans’ Affairs Human Research Ethics Committee.
Results
The study cohort included 10 318 Vietnam veterans with service-related musculoskeletal pain disability. Ninety-nine per cent of study participants were men and lived in the community (Table 1).Over half of the cohort had PTSD (57.3%).Although all study participants had an accepted service-related musculoskeletal pain disability, 39% of those with PTSD and 44% of those without PTSD were not dispensed pain medicines during the study period (Table 2).Veterans with and without PTSD who were dispensed analgesics received a median of two different medicines to manage their pain during the 1 year study period (Table 2).
The most frequently dispensed analgesics, paracetamol (single ingredient product) and paracetamol with 30 mg codeine, were dispensed to more veterans with PTSD than to those without PTSD (Table 2).As a group, opioid analgesics were more likely to be dispensed to veterans with PTSD than those without PTSD; however, the only individual opioid analgesic more likely to be dispensed to those with PTSD compared to those without was paracetamol with 30 mg codeine (Table 2).As a group, NSAIDs were more likely to be dispensed to veterans with PTSD than those without PTSD; however, there was no difference in the proportion of veterans in either group dispensed individual NSAIDs (Table 2).
Table 1 – Vietnam veterans with service-related musculoskeletal pain disability
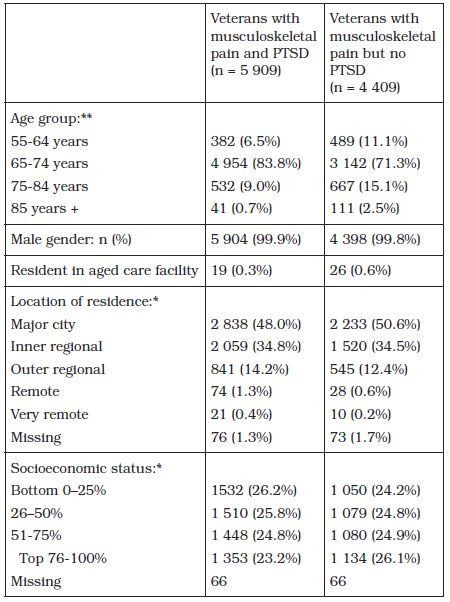
*at 1 July 2015 **No study participants were aged less than 55 years
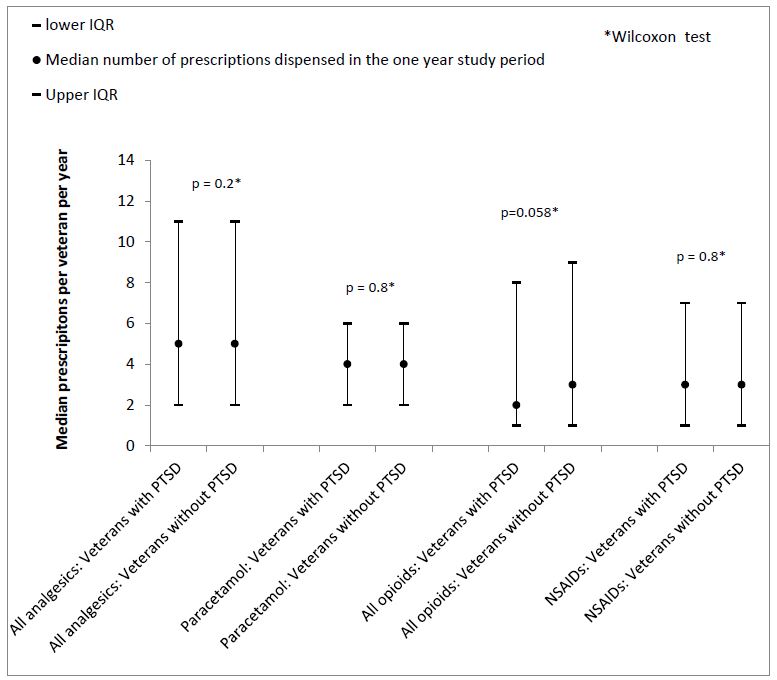
Veterans dispensed analgesics during the study period received a median of 5 (IQR 2-11) dispensings over the 1 year study period. Veterans dispensed paracetamol received a median of 4 supplies over the year. Among veterans dispensed opioid analgesics, the median number of supplies per veteran was 3, and among those dispensed NSAIDs there was a median of 3 supplies over the year. There was no significant difference in the number of dispensings to veterans with PTSD or those without (Figure 1).
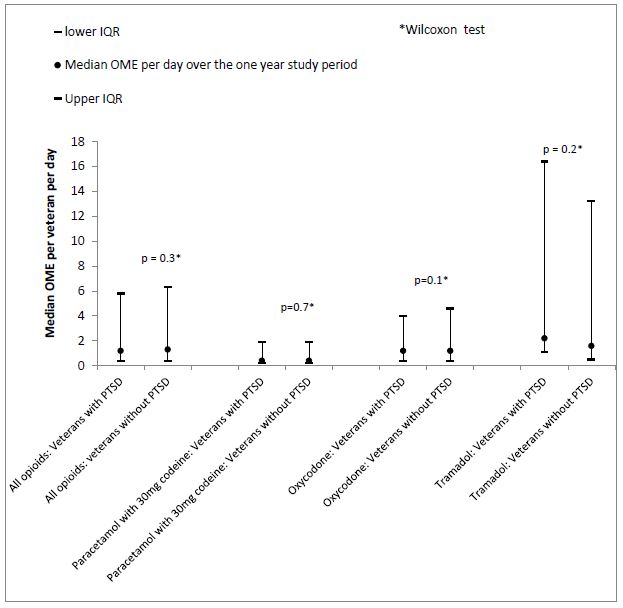
Veterans with PTSD were dispensed a median of 1.2 (interquartile range (IQR) 0.4 – 5.8) OMEs per day over the 1 year study period, which was not significantly different to the volume of opioids dispensed to veterans without PTSD (median 1.3 (IR 0.4-6.3) OMEs per day, p = 0.3) (Figure 2).This is equivalent to the supply of just over three packs of morphine 5 mg tablets (quantity 28 tablets) over the 1 year period. Paracetamol with 30 mg codeine, oxycodone and tramadol were the most frequently dispensed opioid analgesics. The volume dispensed did not significantly differ between veterans with and without PTSD (Figure 2).
Table 2 – Analgesic medicines used by Vietnam veterans with service-related musculoskeletal pain with or without PTSD
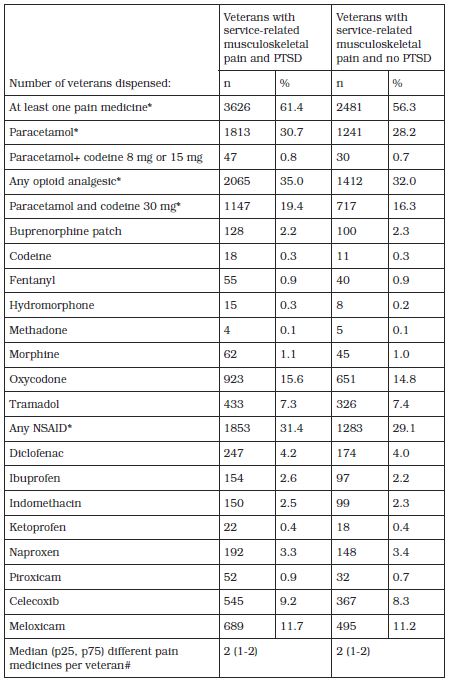
*Chi-square analysis, df=2 for all comparisons. Statistically significant difference in the per cent of veterans with/without PTSD dispensed these medicines: At least one pain medicine p < 0.0001; Paracetamol p = 0.005; Any opioid p=0.002; Paracetamol and codeine 30 mg p < 0.0001; Any NSAID p = 0.01 (no statistically significant difference for other medicines) # Wilcoxon test; p=0.8
The Lorenz curve (Figure 3) shows that the overall volume of use of opioids was very similar for veterans with PTSD and without PTSD. Fifty per cent of opioid users (with and without PTSD) accounted for just over 96% of the total volume of opioid use (Figure 3). This indicates that the remaining 50% of opioid users consumed approximately only 4% of the total quantity of opioids dispensed during the study period.
Discussion
The study highlights that not all veterans’ with chronic service-related musculoskeletal pain receive prescription analgesics. Sixty-one per cent of Vietnam veterans who had PTSD and musculoskeletal pain were dispensed analgesics on prescription during the one year period, compared to 56% of Vietnam veterans with musculoskeletal pain but no PTSD. Paracetamol, alone or in combination with codeine 30 mg, were most frequently dispensed and were more likely to be dispensed to veterans with PTSD than those without PTSD.
An earlier study of analgesic use in Australian general practice patients with chronic pain who visited their GP in April/May 2008 or July/August 2009, found that 86% used at least one medicine to manage their pain, most commonly paracetamol (used by 43% of patients who managed their pain with medicines).14 One-third of patients who used medicines used opioid analgesics (including paracetamol + codeine 30 mg) to manage their pain, while 22% used NSAIDs.14 In our study, a total of 3054 veterans were dispensed paracetamol. This is equal to 50% of the 6107 patients who were dispensed analgesics; slightly higher than the prevalence of paracetamol use in the earlier study involving general practice patients. Fifty-one per cent of the veterans dispensed analgesics during the study were dispensed NSAIDs, and 3477 (57%) were dispensed opioids (including paracetamol + 30 mg codeine), both which are considerably higher than the prevalence of use among general practice patients with chronic pain. The majority of patients in the general practice study were aged 64 years or under and prevalence of pain increased with age.14 The higher prevalence of use of opioid analgesics and NSAIDs in the study population may reflect the older age of the population, as a previous Australian study also showed an increase in opioid use with increasing age.15
Figure 1 – Median number of analgesic prescriptions per veteran over the one year study period
International research has found that veterans with PTSD are more likely to use opioid analgesics, and are more likely to use them at high doses than those without PTSD.8 In the US study, 17.8% of veterans with PTSD were dispensed opioid analgesics compared to 11.7% of veterans with a mental health condition but not PTSD and 6.5% of veterans with no mental health diagnoses.8 In our study, a higher percentage of veterans with PTSD than those without PTSD were dispensed opioid analgesics (35% v 32%); largely due to greater prevalence of use of paracetamol with 30 mg codeine in the PTSD group. However, there was no significant difference in the volume or number of opioid analgesic prescriptions dispensed to veterans with or without PTSD over the study period. The veterans in the study who were dispensed opioids received a median of 1.2-1.3 OME per day for the duration of the study period. This is equivalent to enough morphine to take the minimum recommended dose for chronic non-cancer pain (5 mg twice daily)7 for between 6 and 7 weeks, or 3 to 4 standard packets (each containing 28 tablets) of morphine 5 mg tablets. Opioid analgesics are recommended to be used short-term for musculoskeletal pain7 and our results indicate that, for most Vietnam veterans with service-related musculoskeletal pain disability, short-term use of low-range doses is the norm.
The average daily dose of opioid analgesics dispensed to veterans in our study was much lower than the doses reported in an international study involving veterans. A study involving 141 029 American veterans who served in Iraq or Afghanistan who were diagnosed with pain, found that veterans in the highest quintile of opioid analgesic dose received a dose equivalent to 33 mg of morphine daily or higher.8 By contrast, in our study, veterans in the highest quartile of use were dispensed doses equivalent to 8 mg per day or higher. This difference may be explained, at least in part, by differences in the study methodology: the American study required participants to use opioids continuously for at least 20 days,8 whereas there was no minimum duration of opioid use for patients in our study. In addition, the age and gender of study participants were markedly different. Eleven per cent of participants in the American study were female and 58% were aged under 30 years, compared to over 99% male and all participants aged 55 or over in our study. Other studies have shown that prevalence, dose and duration of opioid use varies by age and gender.15 A national practice improvement intervention involving Australian veterans and their prescribers, aiming to improve the use of medicines for musculoskeletal pain, may have also contributed. This intervention advocated for the use of non-medicine management options where possible, and recommended that opioid analgesics should only be prescribed short-term, at doses lower than those used for managing cancer pain and only after careful consideration of alternative management options. Differences in severity of pain between the two study populations may also have contributed; however, information relating to pain severity is not recorded in our dataset.
Figure 2 – Median OME per veteran per day over the one year study period
Our study identified supply of prescribed analgesics; we were unable to identify the use of analgesics purchased over the counter without a prescription. It is possible that some veterans who were not dispensed prescription analgesics during the study period purchased over-the-counter paracetamol or NSAIDs to manage their pain. It may be that the prevalence of use of analgesics like paracetamol and some NSAIDs, which are available over the counter without a prescription, is higher than reported in our study. However, the prevalence of use of analgesics such as opioids or paracetamol with codeine 30 mg, which are only available via prescription, is likely to be an accurate representation of the prevalence of use in this patient population due to complete capture of data in our dataset. In addition, the high prevalence of use of paracetamol and NSAIDs in our study compared to the general practice chronic pain population indicates that we are unlikely to have underestimated use to a large extent.14 A strength of our study is the use of OME to measure opioid doses. This allows a more accurate comparison of doses for the different opioids than other measures such as the defined daily dose (DDD), which can lead to under or over-estimation of opioid doses actually taken by patients.15 In addition, there is complete capture of prescription medicines dispensed to veterans in our dataset, with no loss to other insurance services. This means that we are more likely to have complete capture of the population of veterans with chronic musculoskeletal disability than international studies, where veterans may have received health care or medicines from other sources and so do not appear in the claims data used. A limitation of our study is our inability to adjust for pain severity because this information is not recorded in the dataset. It may be that some of the veterans in our study who had a record of a musculoskeletal pain-related disability were not dispensed analgesics because they were no longer experiencing pain.
Conclusion
Our study has highlighted that not all veterans with service-related musculoskeletal pain receive prescription analgesics. Among veterans who do receive prescription analgesics, those with PTSD are more likely to receive paracetamol alone, paracetamol with 30 mg codeine or NSAIDs than those without PTSD. For those dispensed opioid analgesics to manage their pain, there was no significant difference in the amount of opioid dispensed to veterans with PTSD compared to those without. Unlike international studies, problematic use of long-term, high-dose prescription opioids was not common in our study cohort.
Corresponding author: Lisa Kalisch Ellett lisa.kalisch@unisa.edu.au Authors: L Kalisch Ellett1, N Pratt1, E Roughead1 Author Affiliations: 1 Quality Use of Medicines and Pharmacy Research Centre, School of Pharmacy and Medical Sciences, University of South Australia






