Alcohol consumption in military populations
There is a long tradition of drinking in military forces. Alcohol has been used to motivate soldiers and manage stress throughout history with many of today’s rituals and ceremonies having their foundation in that past. Ritual and ceremony are an important part of defence cultures providing context and motivation for operational success. Values such as comradeship and commitment contribute to the military culture as does a focus on the importance of team cohesion. Social activities provide the opportunity for the development of team cohesion and allow for debriefing with colleagues in a semi- work environment. Military messes and clubs have been established for these purposes and traditional rituals and behaviours involving heavy drinking in mess environments continue despite official policy in many defence forces banning them1,2,3.
Research confirms that heavy drinking is endemic in western militaries. In the UK and the USA alcohol consumption rates in military personnel exceed those of civilian populations across all age groups1,4. Military leaders are aware of the negative impact that excessive drinking has on the health of their populations, the reputation of armed forces and military capability1,2,3. Research into patterns of alcohol use will enable safe drinking interventions to be targeted at those groups most at risk.
While in general defence personnel consume alcohol at higher rates than civilians, there are certain military subgroups that stand out as heavy drinkers4,5. Young, single males of low educational achievement and lower rank drink significantly more than older people in defence forces and more than young civilian males1,3,4. Young military females drink at higher rates than other military women and more than women in the general population with one study finding that this group binge drink at rates that are even higher than young men in the civilian population4. Personnel who serve in combat units drink more than personnel who perform combat support and combat service support roles. Members who hold positions in medical and welfare units drink the least of all military personnel. However, even these people drink more than their colleagues in the civilian sector4.
Servicemen and women who have deployed on operational missions are heavier drinkers than those
who have not served overseas4,5,6. A longitudinal study undertaken in the UK found alcohol consumption in both deployed and non-deployed personnel increased during a period of significant military commitment for the British Armed Forces. However, the increase was greater for those who had deployed and even higher for those who had been exposed to traumatic events6. It is known that patterns of heavy drinking continue for veterans of deployments long after their retirement from service5 but there is a reluctance for people to seek help for problems associated with drinking while they are still in uniform due to stigma and a perceived and sometimes warranted concern that the impact of seeking help may have on their careers3.
Alcohol consumption in nursing
Nursing is a stressful profession7. Studies on the health and wellbeing of nurses have found an association between reported low levels of health and work stress8,9. Stress on nurses can lead to lost productivity through time off work, increased staff turn-over and nurses presenting to work when sick. Presenting to work when sick can affect performance, have a negative flow-on effect for colleagues and increase the risk for patients10.
Occupational stress in nursing is common11,8. McGrath, Reid and Boore11 found that complex organisational structures, frequent changes, environmental risk and high stress compound challenges for nurses’ professional and psychological wellbeing. Older and experienced nurses have been found to experience more stress than younger colleagues with this stress negatively impacting upon nurses’ motivation and job satisfaction9. These factors can then lead to burn-out12 and ultimately attrition for nurses7. Stress therefore has significance for the maintenance of the nursing workforce and the delivery of healthcare.
The ways in which nurses manage their own health has an impact upon patients13. In a study conducted in the UK, Callaghan13 found nurses’ beliefs in the value of health practices, and the extent to which nurses apply health behaviours in their own lives translates into how readily the same nurses are likely to raise associated health-related behaviours with patients. Additionally, nurses who do not demonstrate healthy behaviours are poor role models for patients14.
Despite the ongoing high levels of stress experienced by the profession, only recently has a body of evidence begun to develop that examines the relationship between stress and the health behaviours of nurses. The link between stress and alcohol is recognised,15 however little research is available to demonstrate a link between nurses using alcohol and experiencing stress. Researchers report that nurses’ alcohol consumption rates mirror those of matched populations7. However, nurses who do drink to excess may be unlikely to be challenged in the workplace about their drinking or to seek help voluntarily due to stigma and possible repercussions on their careers16,17.
Alcohol consumption in military nurses
Stressors experienced by nurses in the civilian sector may be compounded for nurses who serve in the military. Pressure to maintain physical fitness, military duties additional to those of nursing, and the challenges encountered while serving on operational missions all contribute to stress18. Operational deployments are known to pose risk to psychological wellbeing for all personnel, but for nurses the risk may be increased with challenges posed by moral dilemmas when mission goals conflict with professional values19. Griffiths and Jasper18 note that in a cohort of British military nurses, this dichotomy was able to be reconciled. However an American review of the psychological impact of moral distress on military nurses found them to be at particular risk, a risk that requires addressing to prevent ongoing negative effects20.
Emotional exhaustion is common among military nurses18. Social dislocation associated with postings, power disparities related to rank, and exposure to traumatic events have been found to be contributing factors17. While research points to operational service increasing the military nurse’s risk of work- related stress18,19,20, there is evidence to suggest that nurses employed in garrison settings can also experience significant stress. An American study found nurses working in a static military hospital in the United States suffered higher levels of emotional exhaustion than nurses serving on operational missions overseas21. These findings were related to those at home being required to carry out officer responsibilities additional to nursing duties; nurses on deployment performed nursing functions only. Many defence forces, including New Zealand and Australia, recruit registered nurses exclusively into their officer corps. Responsibilities that come with officer rank, irrespective of the profession of the service person, are known to increase the complexity of the employment context22 which in turn, increases stress23.
There has been little research into the drinking patterns of military nurses. Examination of alcohol use in other military cohorts may have some application to military nurses, as might alcohol consumption rates in civilian nurse populations. However, military nursing places unique demands upon those who serve which may impact differently upon how this group of nurses drink. The aim of this study was to explore the drinking behaviours and the alcohol consumption for this group of nurses.
Materials and methods
Design
Data for this study was drawn from the Nurses and Midwives e-Cohort Study (NMeS). The NMeS is a web-based longitudinal cohort study comprised of nurses and midwives from the United Kingdom and Australia and nurses only from New Zealand, recruited for the study between April 2006 and March 200824. Demographic, employment and health information was collected to elicit how the impact of the interrelationship between these factors affects the overall health and wellbeing of nurses and midwives. Further information about the NMeS can be found in Huntington et al.24 and Schluter et al.7.
Participants provided demographic information, professional classifications and employment data at registration. Three surveys were conducted on the study themes of Staying Healthy and Work/Life Balance. The first survey coincided with recruitment and registration, the second survey was held between the 30 August 2008 and 26 September 2009, and the third between May 2010 and May 201124. This sub- study examining the alcohol consumption of military nurses is a cross-sectional analysis of information taken from the second survey.
Ethical approval
Confidentiality was maintained through the allocation of personalised identification codes. There is strictly limited access to participants’ personal information in accordance with ethical requirements. Ethical approval was provided by the University of Queensland Behavioural and Social Science Ethics
Review Committee (2005000696) and the Massey University Human Ethics Committee (Southern B application 05/71).
Participants
To be included in this study, participants were required to be registered nurses serving as enlisted members of the United Kingdom, Australian or New Zealand Defence Forces, and have been working in a defence facility at the time the second survey was conducted. Civilian nurses working in defence establishments were excluded as were registered nurses who were in the military at the time of the survey but not employed in nursing roles. A number of nurses who identified themselves as members of a defence force when registering for the NMeS failed to respond to invitations to engage with the second survey. This may be explained in part by defence nurses being posted to new locations which can involve a change in email address, or by overseas deployment where internet access can be problematic.
Measures
Instruments used in the NMeS comprise of a range of internationally validated research questionnaires that collectively cover the study themes. Questions related to alcohol consumption were derived from the Food Frequency Questionnaire developed by Willett et al. (as cited in Schluter et al.7) and sought to determine drinking/teetotaller status, change in drinking status, the number of days per week participants consumed alcohol and the number of standard drinks consumed on drinking occasions. Responses were assessed using the recommendations of the New Zealand Health Promotion Agency (HPA) for reducing long-term health risks associated with drinking that are based on research commissioned by the Agency25. Table 1 describes these recommendations as they are presented by the HPA’s “Drink Check” brochure26.
Table 1 HPA safe drinking recommendations for reducing long-term health risks26
| Females | Males | |
| Frequency | Drink no more often than 5 days per week | Drink no more often than 5 days per week |
| Numbers of standard drinks per week | No more than 10 | No more than 15 |
| Number of standard drinks per occasion | No more than 2 | No more than 3 |
Guidelines for reducing the risk of long-term harm from alcohol consumption in the UK and Australia are similar to those in New Zealand. The UK government’s guidelines state that men should not regularly exceed three to four units of alcohol per day and women should not exceed two to three27. Australian guidelines for reducing the risk of alcohol- related harm over a lifetime recommend neither men nor women drink more than two standard drinks on any day28. The New Zealand guidelines were selected for this research based on their similarity with those of Australia and the UK, and with the authors’ familiarity with the New Zealand version.
Unsafe drinking is defined by the HPA as when an individual drinks more often than five days per week or when a female consumes in excess of two standard drinks on any drinking occasion, three for males. In addition, the HPA assesses females as falling into a category of unsafe drinking if they consume more than 10 standard drinks per week. For males this is if they drink in excess of 15 standard drinks in a week. As weekly alcohol consumption rates were not established in the survey, these were determined by multiplying the number of standard drinks individuals consumed on drinking occasions by the number of days they drank each week.
Statistical analysis
All data was processed using SPSS version 21 (SPSS, Chicago, IL, USA). Descriptive, frequency and exploratory analyses were undertaken using variables categorised as nominal, ordinal or categorical. Tests of significance were not undertaken as the cohort was not large enough for generalisations to be made to wider defence nurse communities.
Table 2 Defence nurses’ drinking patterns data Total N=44 Males n=15 Females n=29
| All | % | Male | % | Female | % | ||
| Current drinker | No | 3 | 6.8 | – | – | 3 | 10.3 |
| Yes | 40 | 90.9 | 14 | 93.3 | 26 | 89.7 | |
| Missing | 1 | 2.3 | 1 | 6.7 | – | – | |
| History of drinking | Have never drunk | 1 | 2.3 | – | 100.0 | 1 | 3.4 |
| I don’t drink now but I | 2 | 4.5 | – | 2 | 6.9 | ||
| have in the past | |||||||
| I drink now and I have in the past | 41 | 93.2 | 15 | 26 | 89.7 | ||
| Frequency of drinking | Never | 4 | 9.1 | 1 | 6.7 | 3 | 10.3 |
| 1 day per week | 8 | 18.2 | 2 | 13.3 | 6 | 20.7 | |
| 2 days per week | 7 | 15.9 | 2 | 13.3 | 5 | 17.2 | |
| 3 days per week | 11 | 25.0 | 5 | 33.3 | 6 | 20.7 | |
| 4 days per week | 2 | 4.5 | – | – | 2 | 6.9 | |
| 5 days per week | 3 | 6.8 | 1 | 6.7 | 2 | 6.9 | |
| 6 days per week | 3* | 6.8* | 1* | 6.7* | 2* | 6.9* | |
| Every day | 2* | 4.5* | 1* | 6.7* | 1* | 3.4* | |
| Missing | 4 | 9.1 | 2 | 13.3 | 2 | 6.9 | |
| Total who drink more than 5 days per week | 5* | 11.3* | 2* | 13.4* | 3* | 10.3* | |
| Number of drinks consumed in a session | None | 4 | 9.1 | 1 | 6.7 | 3 | 10.3 |
|
1711 | 38.625.0 | 54 | 33.326.7 | 127 | 41.424.1 | |
| 3 drinks | 6 | 13.6 | 4 | 26.7 | 2* | 6.9* | |
| 4 drinks | 4* | 9.1* | – | – | 4* | 13.8* | |
| 5 drinks | 1* | 2.3* | – | – | 1* | 3.4* | |
| 6 drinks | 1* | 2.3* | 1* | 6.7* | – | – | |
| Total who drink more than recommended daily limit (no more than 3 for males, no more than 2 for females) | 8* | 21.9* | 1* | 6.7* | 7* | 24.1* | |
| Total who consume more drinks than recommended weekly limit (no more than 15 for males, no more than 10 for females) | 7* | 15.9* | 2* | 13.4* | 5* | 17.1* | |
* indicates unsafe drinking as per HPA guidelines
Results
Forty four military nurses met the inclusion criteria of which 15 were male and 29 female. Twenty six nurses held nursing registrations in Australia, 11 were registered in New Zealand and five in the United Kingdom. The remaining two eligible nurses failed to respond to this question. Five nurses drank more than 5 days per week and 8 consumed more than the recommended daily limit for their gender. One male nurse drank in excess of daily recommendations while 7 females exceeded their safe daily consumption rates. It was found that 7 of the cohort consumed more than their recommended weekly limit; 2 males and 5 females. Table 2 describes the breakdown of drinking patterns.
Dates of birth were elicited at NMeS registration with nurses’ ages calculated from the date of the closure of Survey 2. Relationships between nurses’ ages and the mean number of drinks consumed per day, numbers of drinking days per week and number of drinks consumed per week were calculated. Participants were also grouped into categories in accordance with their decade of life. Relationships between decades of age and alcohol consumption variables were then calculated.
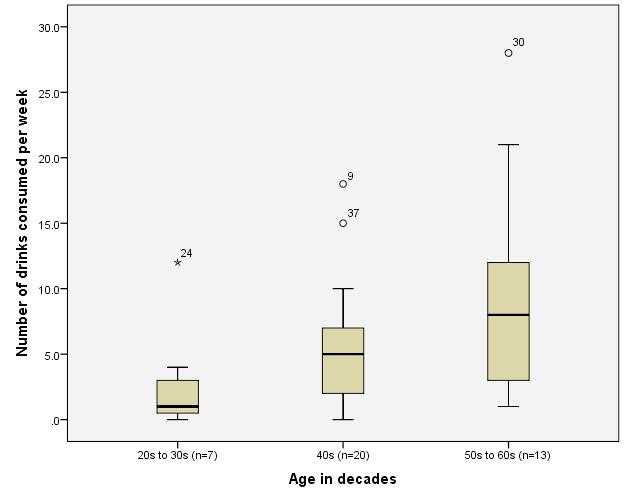
The median number of drinks consumed in a session for each age group ranged between 1 and 2, however a maximum of 6 drinks were reported for nurses in their forties. The median number of drinks consumed per week ranged between 0.5 drinks for nurses in their thirties up to 16.5 for the 2 nurses in their sixties. The maximum individuals reported drinking per week was by nurses in their sixties followed by those in their fifties then nurses in their forties. Nurses in their fifties and sixties drank every day of the week more often than their younger colleagues. Nurses in their twenties drank at the most, 3 days a week. The results of the frequency of drinking and the median and maximum numbers of drinks consumed per day along with the median and maximum numbers of drinks consumed by each age group per week appear in Table 3. Figure 1 illustrates how the number of standard drinks consumed per week increases with age.
Table 3 Numbers of drinks consumed by nurses grouped by decades of age
| Decade of age | Number of drinks consumed per week | Number of drinks consumed per day | Frequency of drinking -days per week. |
| Twenties Number of cases in group | 3 | 3 | 3 |
| Maximum | 12 | 4 | 3 |
| Minimum | 1 | 1 | 1 |
| Median | 2.000 | 2.000 | 1.000 |
| Thirties Number of cases in group | 4 | 6 | 4 |
| Maximum | 4 | 1 | 4 |
| Minimum | 0 | 0 | 0 |
| Median | .500 | 1.000 | .500 |
| Forties Number of cases in group | 20 | 20 | 20 |
| Maximum | 18 | 6 | 6 |
| Minimum | 0 | 0 | 0 |
| Median | 5.000 | 2.000 | 2.500 |
| Fifties Number of cases in group | 11 | 13 | 11 |
| Maximum | 21 | 4 | 7 |
| Minimum | 1 | 1 | 1 |
| Median | 8.000 | 2.000 | 3.000 |
| Sixties Number of cases in group | 2 | 2 | 2 |
| Maximum | 28 | 4 | 7 |
| Minimum | 5 | 1 | 5 |
| Median | 16.500 | 2.500 | 6.000 |
| TotalNumber of cases in group | 40 | 44 | 40 |
| Maximum | 28.0 | 6 | 7 |
| Minimum | 0 | 0 | 0 |
| Median | 4.500 | 2.000 | 3.000 |
Figure 1 Age and number of drinks consumed per week
Discussion
While this study into the drinking patterns of defence nurses is small, there are some indicators that may be cause for concern. Some nurses in the study who were older drank more alcohol more frequently than younger nurses. The older nurses also reported drinking to unsafe levels more than younger nurses. This is particularly the case for nurses in their fifth decade of life but also pertains to a lesser extent, to nurses in their forties. Nurses in their sixties drank the most in all measures. Findings that older nurses in this study drink more than younger nurses is unexpected and is the inverse of previous studies where unsafe drinking has been found to be significantly more common in younger military people, both male and female. Factors that may contribute to older nurses’ increased alcohol consumption in relation to their younger colleagues revolve around the length of time nurses serve and the nature of that service.
The longer nurses are exposed to the defence culture the more likely they may become inculcated to military norms and values. Like other personnel, the military nurse operates in an environment where their work is blended with their personal life and where alcohol is readily available and accepted as part of that life29. Socialising with personnel who use alcohol as a means of managing stress will expose defence nurses to the extremes of these norms and the association between alcohol consumption and operational deployment will become more evident the more time they spend in that environment.
Older military nurses are more likely to have deployed than younger nurses as there are more opportunities for deployment over time. Longer serving nurses may have undertaken a range of operational tours that could involve peacekeeping and disaster response as well as combat missions. All occupational groups are reported to use alcohol to manage stress that results from deployment with those who serve in medical units not being exempt4. Military nurses most frequently serve in medical units.
Alcohol consumption has been found to increase most significantly over time in those who have been exposed to life-threatening traumatic events and those who have experienced hostility from civilians during missions6. However, there has been little research into the stress experienced by military nurses working with those who have been injured as a result of combat, and little into the relationship between military nurses’ stress and alcohol consumption. This area requires research to inform the way ahead for improvements in the health of this group.
Iverson et al.3 note that peacekeeping presents unique challenges where service personnel experience significant frustration associated with their inability to act against human rights violations. Peacekeepers in this study were found to consume alcohol at higher rates than personnel who had deployed on other types of missions. Iverson’s observations about possible causes of the relationship between alcohol consumption and peacekeeping have some resonance with the moral distress experienced by defence nurses when on deployment.
Defence nurses have described moral distress as their inability to practice in accordance with what they believe to be in the best interests of their patients18. Tension can exist between military orders driven by mission imperatives, and nursing judgement. This may result in nurses being compelled to compromise on best practice which in civilian settings has been found to lead to the inappropriate use of alcohol30. Whether military nurses turn to alcohol to deal with moral distress resulting from care rationing on operational missions is yet to be studied.
There are unique challenges for defence nurses seeking help with alcohol-related problems. Military nurses serve in the same units that facilitate and at times provide the care they themselves may require. Concerns surrounding the maintenance of confidentiality and the potential impact upon careers of disclosure of alcohol-related problems are very real for these nurses. There is a danger that if professional boundaries are not respected, line managers may be involved in care provision at the same time as being required to provide information to command about their patients’ individual military effectiveness.
Defence nurses are expected to role model healthy behaviours. Callaghan13 noted that the personal health habits of nurses impacts upon their ability to raise related health issues with their patients. This has significance for defence forces because as a condition of service, military personnel are required to obtain their healthcare through their employer. When military nurses find it difficult to raise issues with patients due to their own health behaviours, the impact may be greater because of a smaller population and smaller number of nurses providing that care. It is of course, incumbent on defence nurses as much it is with their civilian counterparts, to act as role models for their patients.
Defence nurses are a select group of highly skilled health professionals who receive significant investment in their professional development. Any loss or impairment of one of these individuals has the potential to impact disproportionately upon health capability. It takes time to recruit and develop military nurses to the level where they can become operationally effective so vacancies are problematic. Given the nursing profession is facing critical shortages as the general population ages7, strategies are needed to assist military forces to retain and optimise the effectiveness of those nurses already serving.
While alcohol consumption continues to provide a social screen behind which stress management is hidden, the imperative to create and provide safe and acceptable alternative approaches are not there. Any way forward will involve military forces continuing to work to change entrenched drinking cultures, as well as implementing systematic improvements so that stigma and fear of repercussions are no longer barriers to individuals seeking help for alcohol related problems.
At the commencement of this research expectations had been that military nurses would reflect the drinking patterns of their profession rather than those of their employing organisation. In this study, indications are that this group of defence nurses identify more closely with military forces than they do with their profession. This may be confirmation of the effectiveness of defence forces’ efforts to impress their culture on service members or it may perhaps be a reflection of the nature of stress experienced by defence nurses. Military nurse leaders need to appreciate fully the dynamics in operation that may be leading to unsafe drinking in their nursing workforces and ensure that strategies that minimise or mitigate against stress are in place. There is a need for further research to inform these strategies such as a wider survey of a representative sample of defence force nurses.
Study limitations: Given the small numbers of nurses in the survey, no generalisations can be made about the application of the findings in this study to other groups of military nurses. Nurses in their sixties drank the most in all measures; however there were only two nurses in this group which hampers comment about any relationship between these two nurses and others. Additionally, the data is self reported so may not accurately portray alcohol consumption over time.
Conclusion
Issues in this study raise the possibility that unique employment and social conditions in defence forces may, over time, contribute to nurses consuming alcohol in excess of recommended rates. Interdependencies between a culture of heavy drinking, nurses’ health related behaviours and the impact of poor role modelling on patients should be of concern to defence leaders. The health of the wider defence population is influenced by military nurses through their ability to raise health related behavioural issues with their patients and the health of nurses is, of course, affected by their personal drinking patterns. Both effects impact upon defence capability.
While this study is small-scale and therefore cannot be used as a basis for generalisation, it has raised an important issue which, for the health of military nurses and for defence forces overall, needs further exploration.



